Lancet haemat:肿瘤相关静脉血栓风险的临床预测模型
2018-06-07 MedSci MedSci原创
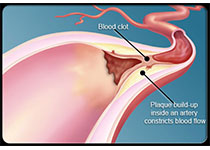
静脉血栓是癌症的一种常见并发症,但静脉血栓形成的风险因人而异,取决于多种因素,包括癌症类型。Ingrid Pabinger等研究人员尝试开发一种用于预测癌症相关静脉血栓风险的临床模型,并进行外部验证。研究人员利用前瞻性研究——维也纳癌症和血栓研究(CATS)队列(1423位患者)的数据建立预测模型。然后在另一个相似的前瞻性多国家研究队列(MICA,832位患者)中验证该模型。此外,研究人员计算C指
研究人员利用前瞻性研究——维也纳癌症和血栓研究(CATS)队列(1423位患者)的数据建立预测模型。然后在另一个相似的前瞻性多国家研究队列(MICA,832位患者)中验证该模型。此外,研究人员计算C指标,比较两组6个月时预测的静脉血栓发生率与实际观察到的血栓累积发生率是否存在出入。
终极版临床预测模型纳入两个变量:肿瘤风险类型(低危或中危 vs 高危 vs 极高危)和D-二聚体浓度。高危或极高危与低危或中危相比,多变量分布风险比为1.96(95% CI 1.41-2.72;p=0.0001);D-二聚体浓度每增加一倍,多变量分布风险比为1.32(95% CI 1.12-1.56;p=0.001)。在CATS和MICA队列研究中,终极版模型的交叉验证的C指标分别是0.66(95% CI 0.63-0.67)和0.68(0.62-0.74)。临床预测模型在两个队列中都得到充分校准。
经外部验证的临床预测模型,仅包含一个临床因素(肿瘤风险分类)和一个生物标志物(D-二聚体),即可预测固体肿瘤患者的静脉血栓风险。该简单模型极大改进了已有的癌症相关静脉血栓的预测模型,并可帮助临床医生筛选可能受益于血栓预防的患者。
原始出处:
Ingrid Pabinger,et al.A clinical prediction model for cancer-associated venous thromboembolism: a development and validation study in two independent prospective cohorts.The Lancet Haematology. June 06,2018.https://doi.org/10.1016/S2352-3026(18)30063-2
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
29
#HAE#
27
#静脉血#
27
#静脉#
33
#预测模型#
37
#EMA#
27