Int Arch Allergy Immunol:在中国中部,8个气源性致敏表皮提取物也许检测过敏性鼻炎更优组合
2017-09-06 AlexYang MedSci原创
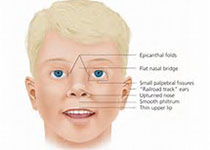
过敏性鼻炎(AR)在中国中部的流行程度增加迅速。皮刺试验(SPT)是确定AR病人过敏原敏感状态的标准工具。由于地理和季节的变化,研究人员在不同的国家和地区观察到了过敏原敏感模式的改变。最近,有研究人员进行了旨在评估在AR病人中,SPT对不同气源性过敏原的反应,并且尝试建立一个过敏原最小组合来检测中国中部敏感病人。从2015年1月到2016年12月,研究人员对同济医院怀疑患有AR的病人进行了19种气
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#过敏性#
30
#ALL#
28
不错的文章值得学习
48
学习了谢谢分享
47
学习了新知识
54
不错的文章值得学习
52