NEJM:NSCLC患者术前两次PD-1成功减少术后复发
2018-04-17 癌度 癌度
如果被诊断为肺癌,但是可以通过手术治疗,这无疑是一件很幸运的事情。临床上以5年未复发作为临床治愈,IA期非小细胞肺癌的5年生存率80%以上,如果是IIIA期患者的5年生存率就下降至20%左右。 多数患者手术之后会经历复发的风险,在手术期间进行以铂类药物为基础的化疗,相比单独手术,生存率仅仅提高了5.4个百分点,但是3级以上的毒副作用超过了60%。 如果在早期肺癌患者中使用PD-1药物,可以增强
如果被诊断为肺癌,但是可以通过手术治疗,这无疑是一件很幸运的事情。临床上以5年未复发作为临床治愈,IA期非小细胞肺癌的5年生存率80%以上,如果是IIIA期患者的5年生存率就下降至20%左右。
多数患者手术之后会经历复发的风险,在手术期间进行以铂类药物为基础的化疗,相比单独手术,生存率仅仅提高了5.4个百分点,但是3级以上的毒副作用超过了60%。
如果在早期肺癌患者中使用PD-1药物,可以增强宿主免疫的抗肿瘤效果,降低肿瘤细胞的异质性。尤其是在患者手术前的新辅助治疗时期使用PD-1,还没有切除的肿瘤病灶可以释放很多抗原,这将激发人体的免疫细胞扩增,这些扩增的免疫细胞将会对微小的转移灶进行压制。
理论上是这样,但事实如何呢?
PD-1抑制剂纳武单抗(nivolumab)用于早期肺癌的术前,可以激发45%的患者免疫系统。研究刚刚发表在新英格兰杂志上。
本次临床试验入组了22名早期非小细胞肺癌,有I期、II期或IIIA期,且可以认为是能够进行手术治疗的病人。使用的剂量为每公斤体重3毫克,每两周一个疗程。在第一次使用药物之后的4周进行手术治疗。所有患者至少接受了一个剂量的PD-1治疗,一名患者发现有小细胞肺癌成分而终止了治疗。
结果发现:纳武单抗在术前使用具有可接受的副作用,并且不会延迟手术时间。
21例入组的患者中,有20例患者的肿瘤完全切除,一名IIIA患者因为气管侵犯而未能手术治疗。第二次PD-1治疗与手术治疗的间隔时间平均是18天。使用PD-1治疗之后进行的影像学检查发现(还没有进行手术切除前),2名患者对PD-1治疗产生了部分应答。18名患者病情稳定,仅仅一名患者病情进展,即疾病控制率为96%。

20名可以评估的患者中有8名患者发生了临床前病理性降期(占比40%)。术后随访的一年中,20名患者中的16名患者没有复发,占比80%。18个月的无复发生存率为73%。

9名患者的切除病灶出现了对PD-1的病理学应答,占比为45%。有3名患者在原发肿瘤中有完全的病理性应答,也就是没有活性的癌细胞了
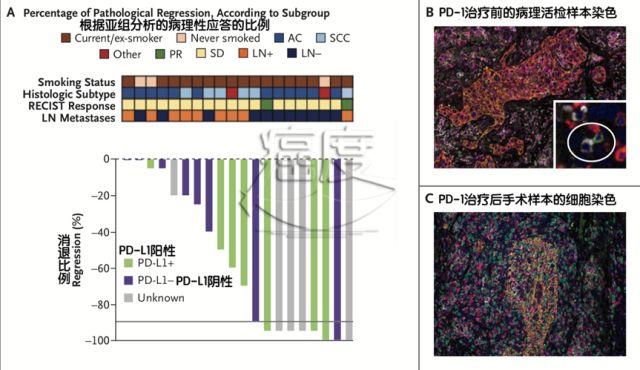
原发肿瘤病灶的病理性消退的比例是65%,尽管有的患者在CT上观察病灶变大了,可能是因为免疫细胞浸润,这就是所谓的假性进展,如上图的78岁的女性患者,虽然CT显示病灶变大了,但那是因为免疫细胞进入病灶,其实病理检查发现癌细胞都死亡了。

在产生病理性反应的原发性病灶中,我们可以看到大量的浸润淋巴细胞和巨噬细胞,这与免疫反应的机制是相符的。
如上图所示,在治疗前有15个患者进行了病灶穿刺评估PD-L1表达情况,不管PD-L1表达阳性还是阴性,其实都可能会对PD-1产生病理性应答。

如上图所示,有12名患者的手术组织病灶进行全外显子组测序,分析肿瘤突变负荷(TMB)的状态。平均每个肿瘤鉴定出了92个基因突变,包含TP53、KRAS、CDKN2A和NOTCH1和RB1。
通过这些患者的测序结果可知,肿瘤病灶的病理反应与治疗前的肿瘤突变负荷(TMB)存在显著的相关性。如果肿瘤突变负荷高,则患者经过PD-1治疗后的病灶残余就小。

如上图所示,PD-1治疗后,可以看到相关T细胞数量增加。本次试验9名可以评估的患者中,8名患者在使用PD-1之后,可在外周血和肿瘤病灶发现免疫T细胞数量增加。
有一例病理上对治疗完全缓解的病人,在使用纳武单抗之后2-4周出现大量可识别原发肿瘤病灶特异性突变的免疫T细胞,而在使用纳武单抗之前从未检测到这些免疫T细胞。
结语
这是一项非常有意义的研究,对于诊断为早期的非小细胞肺癌患者,在手术治疗前打两个疗程的PD-1,这个经济花费也并不是太高,但是可以预见对于术后的复发风险将会有很大的益处。
原始出处:
Patrick M. Forde, M.B., B.Ch., Jamie E. Chaft, M.D, et al.Neoadjuvant PD-1 Blockade in Resectable Lung Cancer.DOI: 10.1056/NEJMoa1716078
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#术后复发#
25
#SCLC患者#
26
简直就是觉得觉得你们什么
42
nvvhjhbvvvvvvvcc
52
可可可可可可可
45
时间就是觉得很好的回答很好
47
#NSCLC患者#
18
经济和方法规划和规范
38