ASCO 2019:Brentuximab vedotin治疗淋巴瘤优势显著,不依赖CD30表达
2019-06-08 良医汇-肿瘤医生APP 良医汇-肿瘤医生
2019年美国肿瘤学(ASCO)年会于美国东部时间5月31日—6月4日在芝加哥举办。作为全球肿瘤领域最为期待的盛会,每年的ASCO年会都会公布多项肿瘤领域重磅研究,讨论当前国际先进的治疗方式和治疗方法。Brentuximab vedotin(以下简称“BV”)是新型靶向CD30的抗体-药物偶联物,研究证实其在多种血液肿瘤中疗效显著。本次ASCO年会公布了两项研究结果,探讨了CD30表达水平与BV治
2019年美国肿瘤学(ASCO)年会于美国东部时间5月31日—6月4日在芝加哥举办。作为全球肿瘤领域最为期待的盛会,每年的ASCO年会都会公布多项肿瘤领域重磅研究,讨论当前国际先进的治疗方式和治疗方法。Brentuximab vedotin(以下简称“BV”)是新型靶向CD30的抗体-药物偶联物,研究证实其在多种血液肿瘤中疗效显著。本次ASCO年会公布了两项研究结果,探讨了CD30表达水平与BV治疗CD30+淋巴瘤疗效关系。
ECHELON-2 (E-2)研究:CD30表达水平与A+CHP疗效
背景与方法:
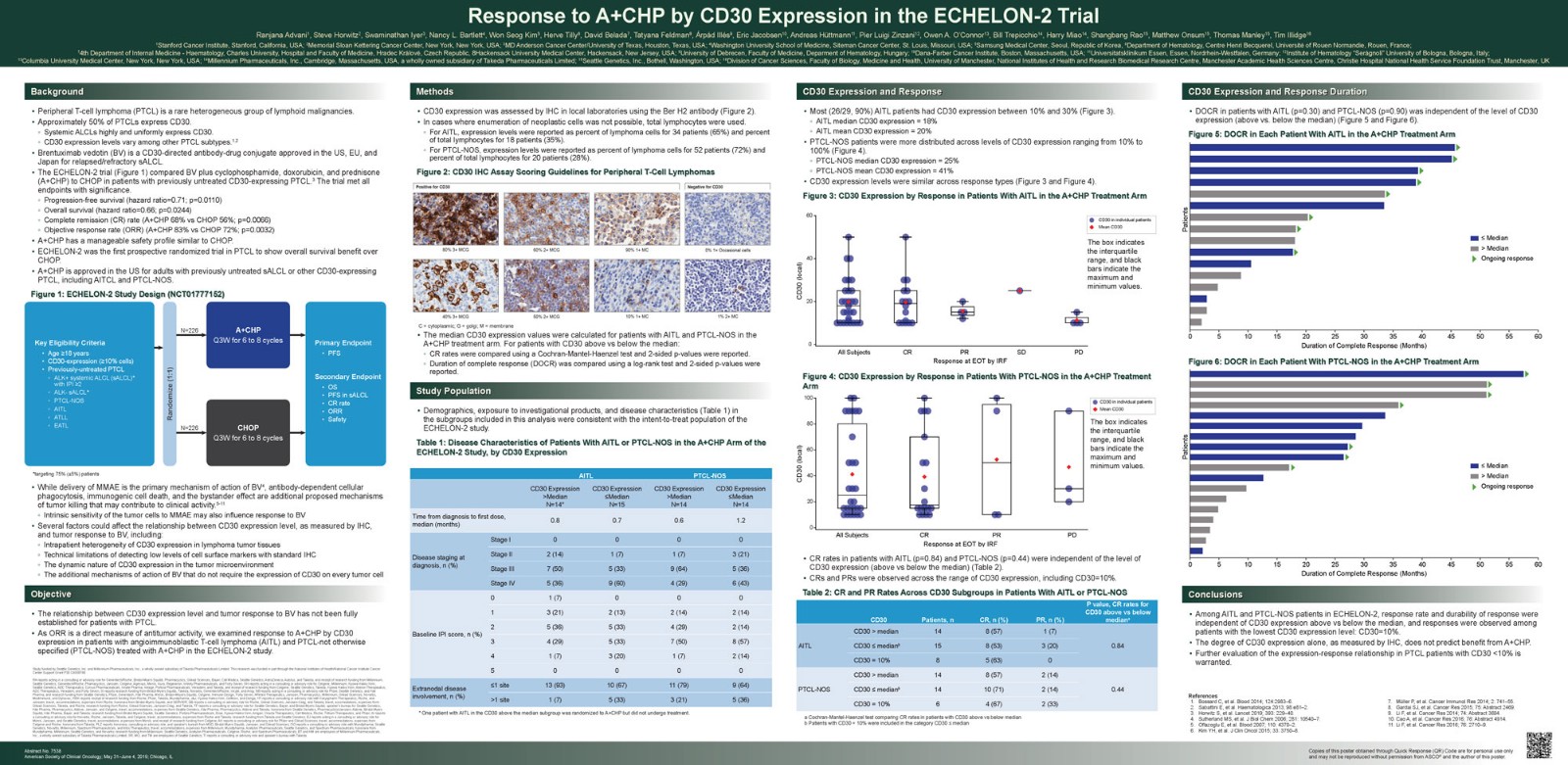
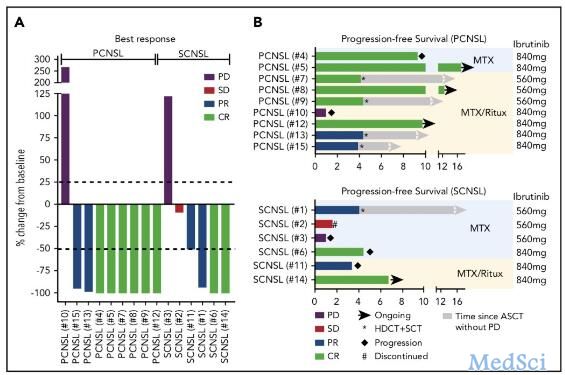
结果:AITL患者中CD30表达水平在10%~30%的占90%(26/29),PTCL-NOS患者中CD30表达水平多在10%~100%。CD30表达水平与AITL和PTCL-NOS患者的DOCR均无明显相关性(P=0.30 AITL;P=0.90 PTCL-NOS,log-rank检验,图1、2),CD30表达水平与AITL患者反应率不存在明显相关性(表1)
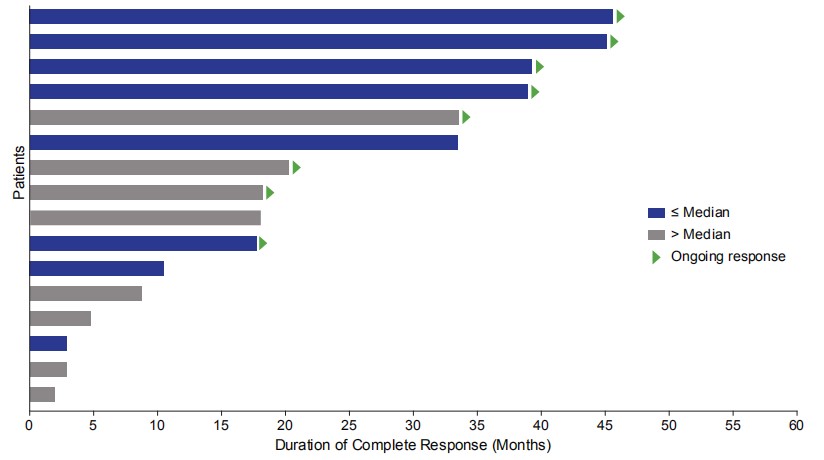
图1. A+CHP治疗组每例AITL患者的DOCR
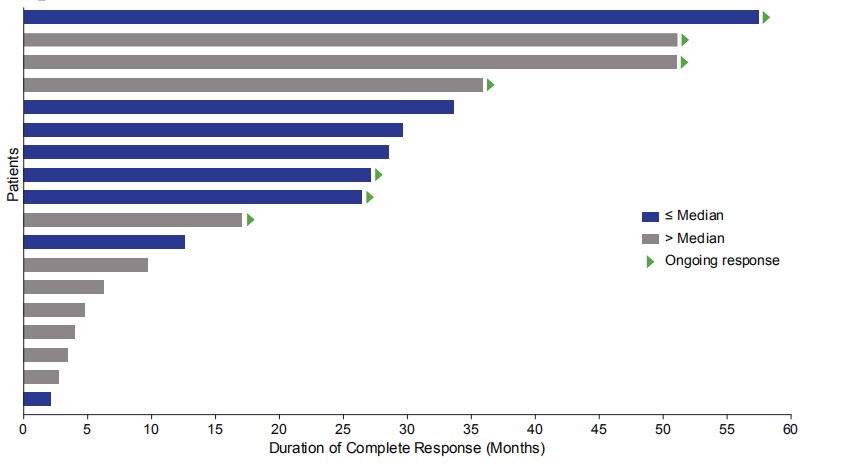
图2. A+CHP治疗组每例PTCL-NOS 患者的DOCR
表1. AITL或PTCL-NOS患者中通过CD30亚组分析的CR和PR率
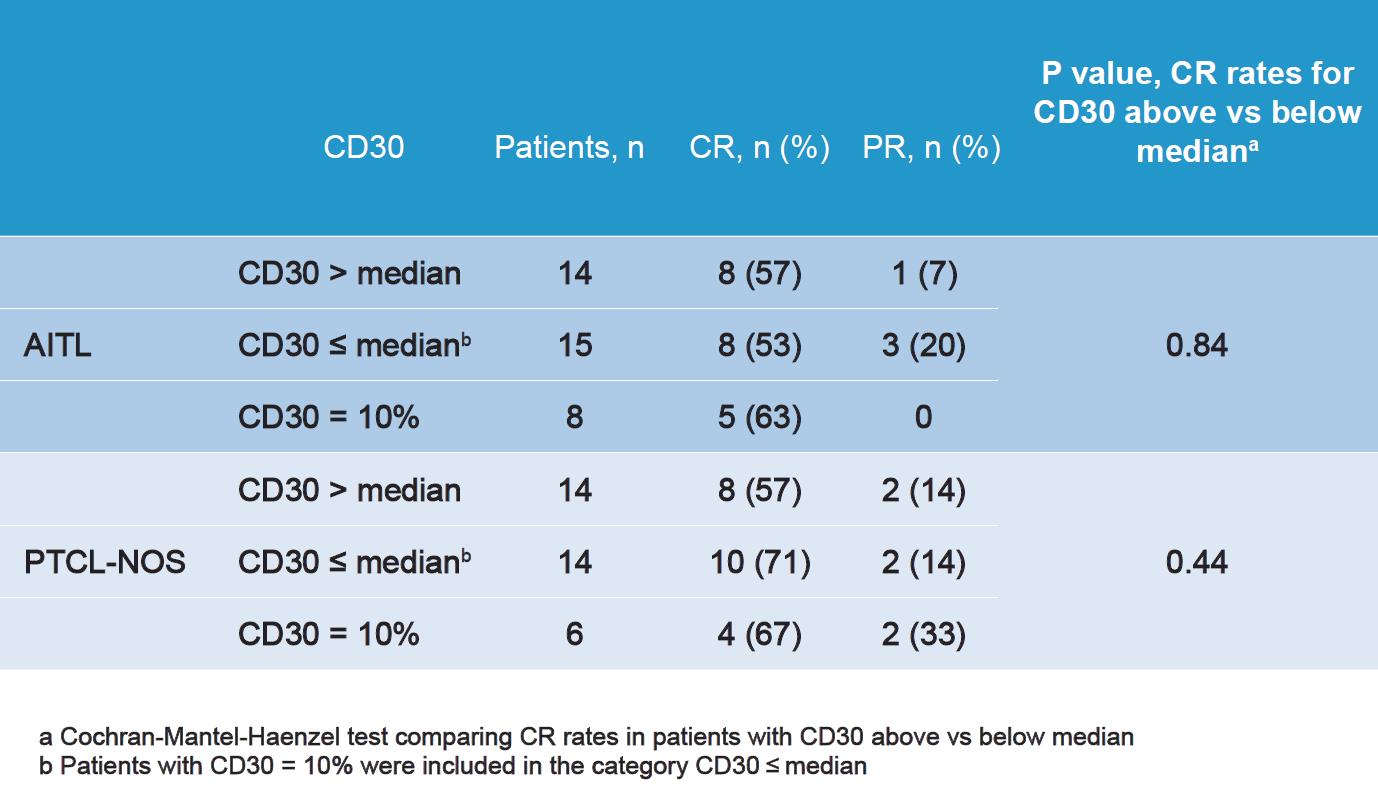
结论:在E-2研究中,由于不同CD30表达水平之间的患者均达到缓解,这就表明无论CD30表达水平高于或低于中间值(或至少10%),A+CHP方案均能有效治疗non-ALCL患者的。研究人员猜想这个结果可能与细胞内和细胞间CD30表达水平的异质性、CD30存在于细胞表面、免疫组化技术限制和BV作用机制复杂有关。后续将在CD30<10%的PTCL患者中进一步评价CD30表达-反应关系。
5项临床试验:CD30表达水平与Brentuximab vedotin疗效
背景与方法:BV是靶向CD30的抗体-药物偶联物,在PTCL、皮肤T细胞淋巴瘤(CTCL)以及B细胞淋巴瘤的多项临床试验中均取得良好疗效。本研究通过分析CD30表达水平以预测BV在上述患者中的疗效。本研究收集来自5项前瞻性临床试验的275例接受BV治疗的PTCL、CTCL和B细胞淋巴瘤患者资料。SGN35-012是一项评估BV联合利妥昔单抗或BV单药治疗难治/复发非霍奇金淋巴瘤(NHL)的临床试验,ALCANZA试验对比了BV和甲氨蝶呤或贝沙罗汀治疗蕈样真菌病(MF)、原发ALCL(pcALCL)疗效。另外3项研究者赞助的临床试验评估了BV单药治疗复发的PTCL、MF和pcALCL疗效(临床试验编号:35-IST-030,35-IST-001,35-IST-002)。采用免疫组化法(肿瘤细胞或淋巴浸润;局部评估)检测CD30表达≥10%,<10%或不可测(0%)的患者CD30表达水平和ORR之间的关系。
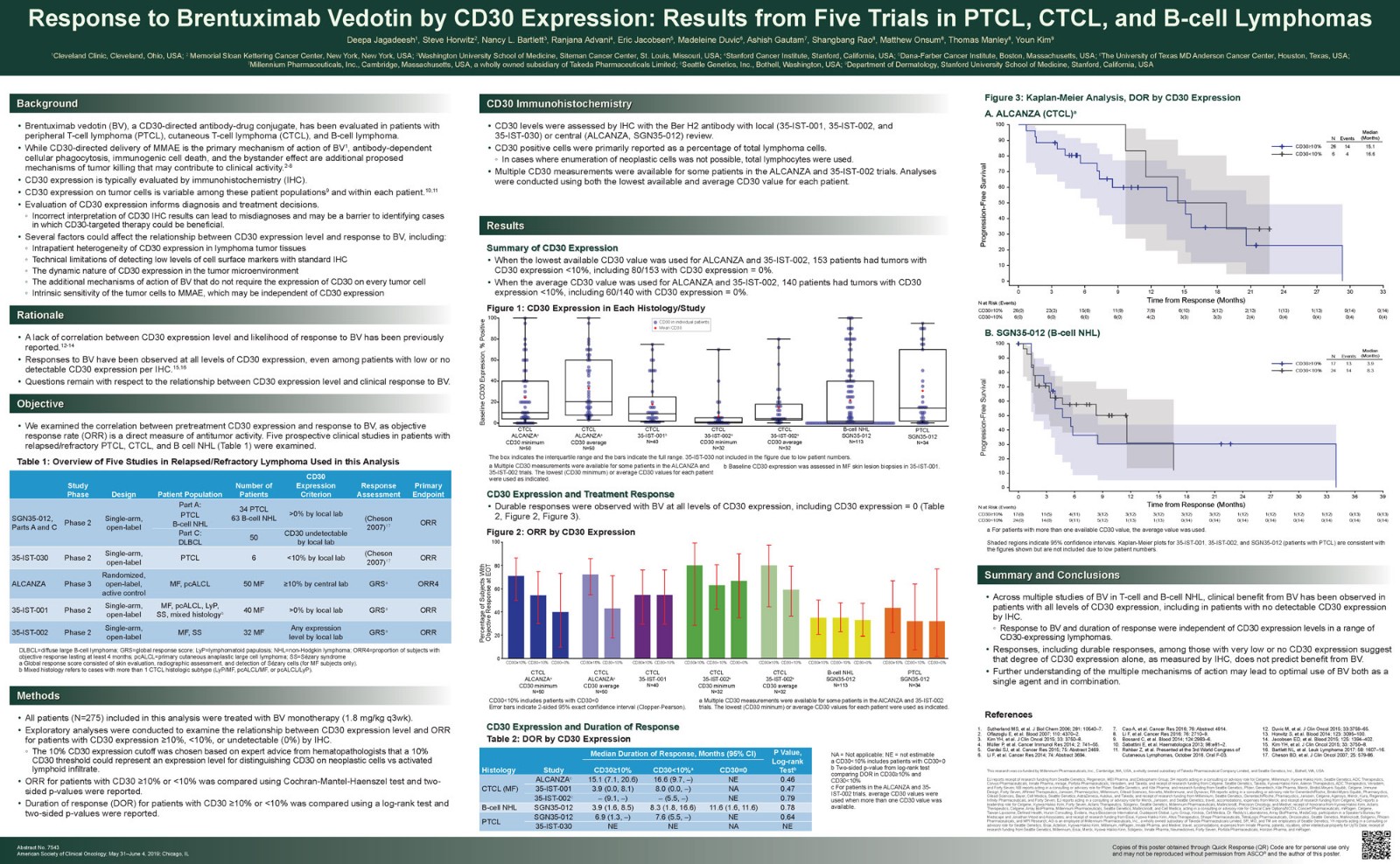
结果:143例患者CD30表达水平<10%,其中58/143例患者CD30水平未测出。包括CD30水平未测出的患者在内,所有CD30表达水平的患者接受BV治疗后均达到了持续缓解。BV治疗后患者CD30表达水平和反应率之间的关系如图3所示,CD30表达水平和反应持续时间关系如表2所示。
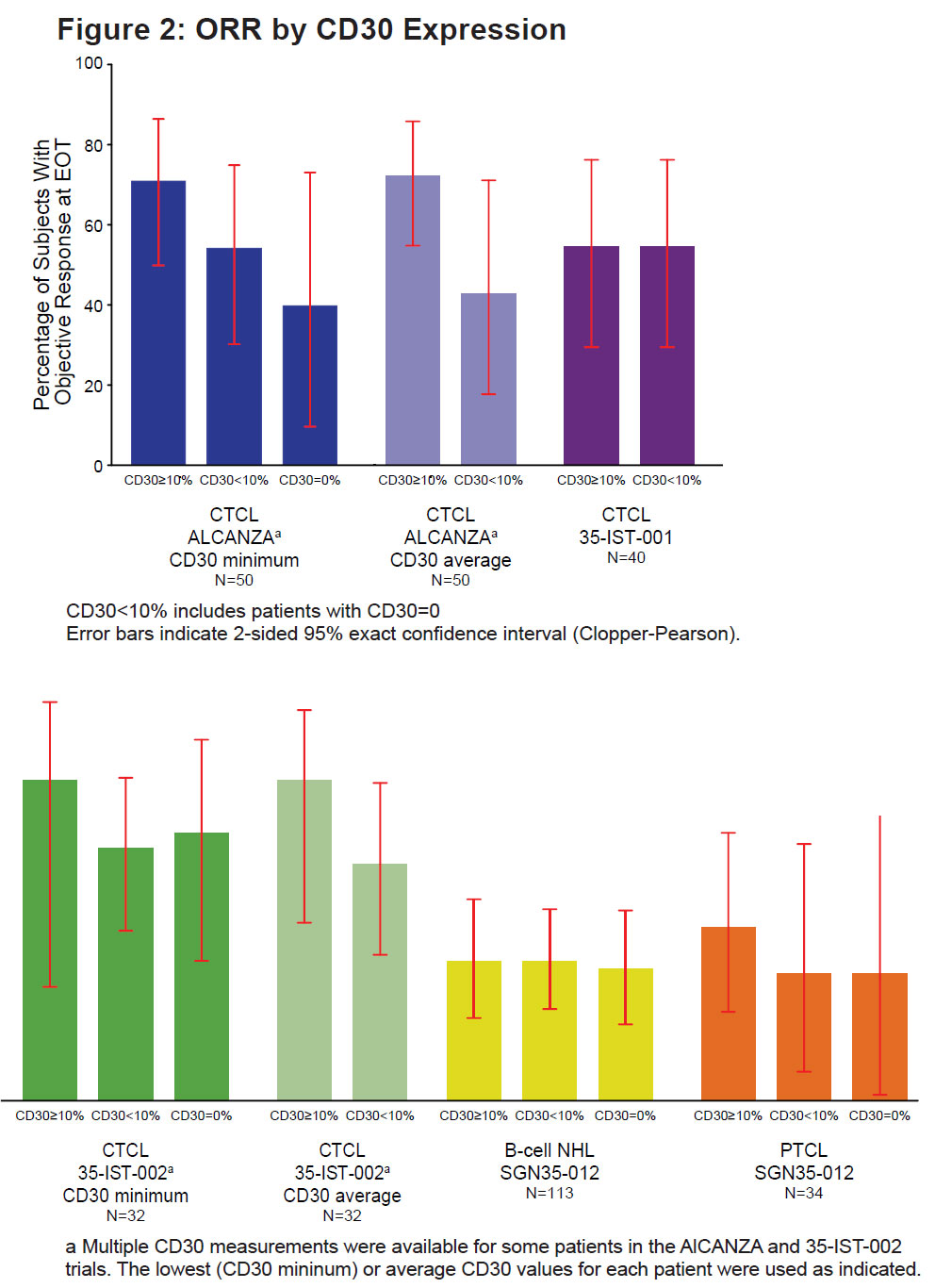
图3. 基于CD30表达的总反应率
表2. 基于CD30表达的反应持续时间
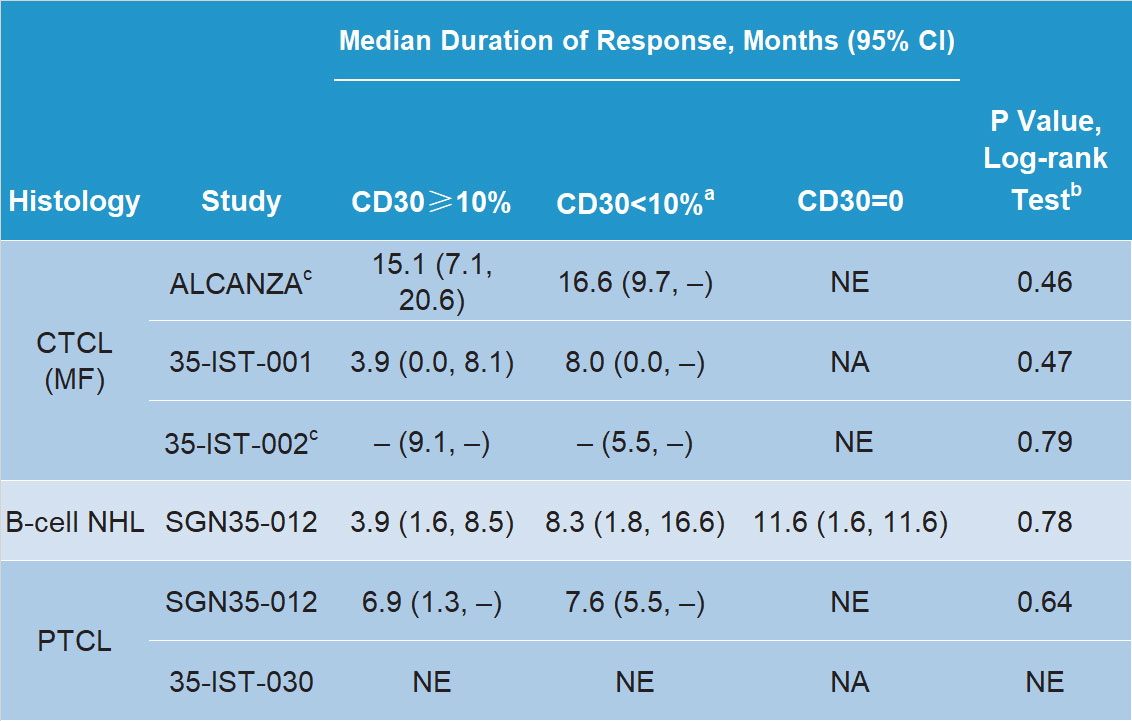
结论:BV治疗T细胞非霍奇金淋巴瘤、B细胞非霍奇金淋巴瘤的上述多项研究结果显示,包括表达水平极低或未测出在内的不同CD30表达水平的淋巴瘤患者接受BV治疗均可达到缓解或持续缓解。无论患者CD30表达水平高低(≥10%、<10%或未测出),BV均表现出良好疗效,这可能与细胞表面CD30表达的动态本质和异质性、免疫组化技术限制以及BV抗肿瘤作用机制复杂有关。
BV治疗淋巴瘤疗效显著,深究其作用机制可为单药或联合用药提供新思路
BV在血液肿瘤中的研究进展非常迅速,在CD30表达的PTCL、CTCL及B细胞淋巴瘤等多种血液肿瘤中均取得良好疗效,并且研究显示CD30表达水平不影响其疗效。截至目前,美国FDA已经批准了BV在霍奇金淋巴瘤和外周T细胞淋巴瘤中的6类适应证。未来通过进一步探索BV作用机制可为选择BV单药或联合应用治疗淋巴瘤提供思路。随着更多研究的开展及深入探索,我们期望BV能带来更多的好消息,造福更多的淋巴瘤患者。
参考文献[1]Advani RH, Horwitz SM, Iyer SP,et al.Response to A+CHP by CD30 expression in the ECHELON-2 trial[J].J Clin Oncol , 2019,37 (suppl; abstr 7538).
[2]Jagadeesh D,Horwitz SM, Bartlett NL,et al.Response to brentuximab vedotin by CD30 expression: Results from five trials in PTCL, CTCL, and B-cell lymphomas[J].J Clin Oncol , 2019,37 (suppl; abstr 7543).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#mAb#
26
#ASC#
22
#CD30#
41
#Brentuximab#
35
#vedotin#
30