AHA 2017:重要实验结果公布:Anacetrapib对新发糖尿病发病及糖尿病患者血管事件的影响
2017-11-18 佚名 国际循环
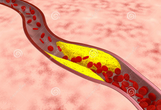
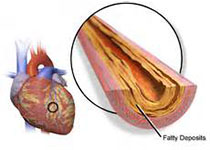
众所周知,糖尿病患者的心血管发病及死亡风险会增加,而采用他汀治疗降低LDL-C可使糖尿病的发病风险增加10%~20%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#结果公布#
32
#血管事件#
31
#ANA#
32
#TRA#
34
#ACE#
27
#TRAP#
37
#AHA#
36
#糖尿病患者#
27
厉害了我的哥不错
62
学习一下谢谢
62