Lancet oncol:Venetoclax用于进行过依鲁替尼治疗的复发性/难治性慢性淋巴细胞白血病的疗效和安全性。
2017-12-13 MedSci MedSci原创
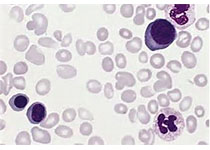
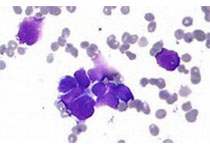
用依鲁替尼靶向Bruton酪氨酸激酶(BTK)疗法改变了慢性淋巴细胞白血病的治疗。然而,难治性/复发性慢性淋巴细胞白血病患者应用依鲁替尼治疗,预后仍然较差。Venetoclax是一种选择性的、口服的BCL-2活性抑制剂,既往用于治疗难治性/复发性慢性淋巴细胞白血病。现有研究人员进行临床试验,评估Venetoclax用于正在采用或已进行过依鲁替尼治疗的复发性/难治性慢性淋巴细胞白血病患者的疗效和安全
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
19
#疗效和安全性#
28
#NET#
23
#Lancet#
31
#复发性#
37
#淋巴细胞白血病#
24
#淋巴细胞#
19
#难治性#
35
学习学习.继续关注
65
学习.
56