第十七届中国介入心脏病学大会(CIT2019)|侯玉清:NSTE-ACS介入治疗的时机与策略
2019-03-30 Gill MedSci原创
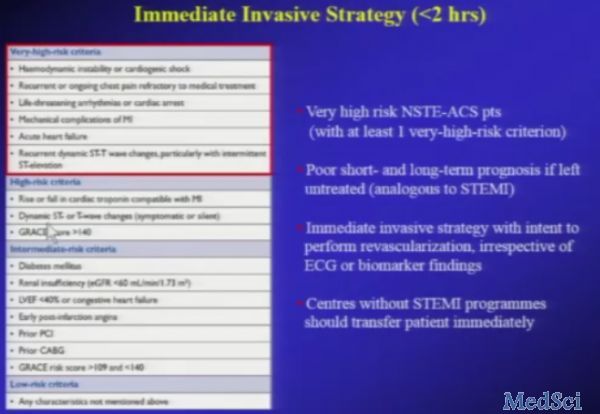
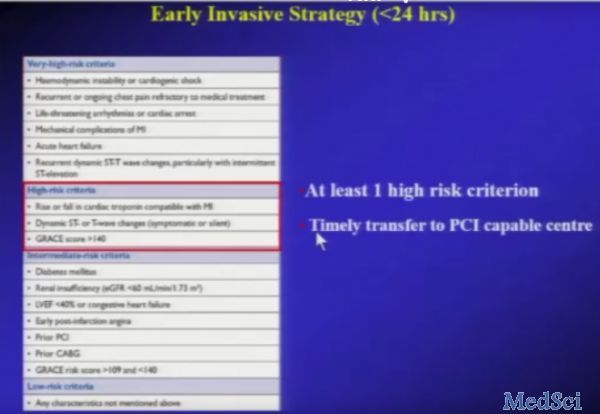
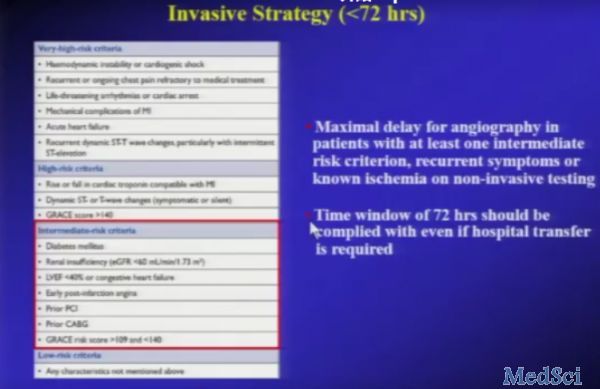
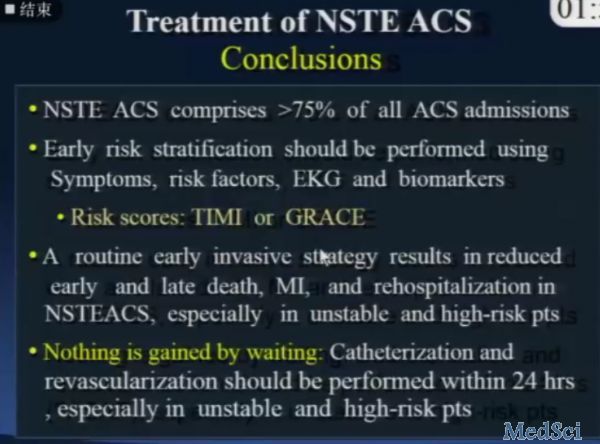
非ST段抬高型急型冠状动脉综合征(NSTE-ACS)行造影可见局部血栓或狭窄,尚存在部分血流。判断ACS主要根据:1.临床典型症状;2.心电图典型表现;3;肌钙蛋白升高。还应注意,心梗三项自2014年起欧洲指南起不推荐用于ACS诊断。目前有大量RCT研究证明,对于ST段抬高型急型冠状动脉综合征(STE-ACS)应该尽早进行介入治疗,此类患者多为中青年;而非ST段抬高型急型冠状动脉综合征(NSTE-
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CIT#
23
#NSTE-ACS#
31
#心脏病学#
25
#NST#
29
#介入心脏病学#
31
谢谢分享学习
62
谢谢分享学习
62
#ACS#
27