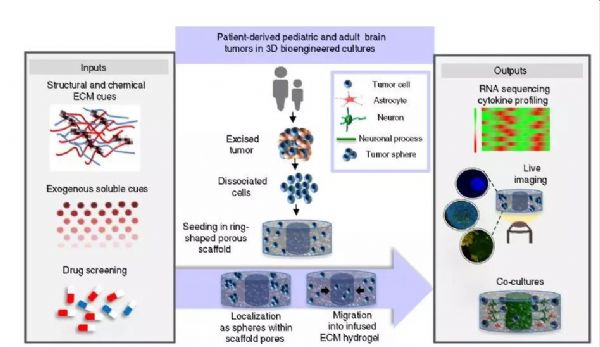
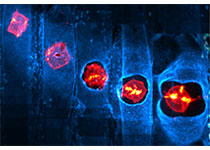
Nat Commun:3D技术模拟大脑微环境,或成脑瘤治疗新突破!
2019-10-09 Eagle 转化医学网
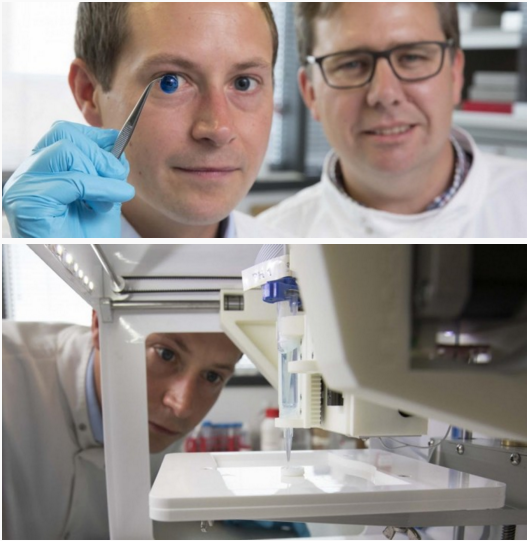
作为当下最火的新兴技术,3D打印的广泛应用可能造就许多跨时代的应用价值。尤其在医疗健康领域中,3D生物打印技术更是为临床医生和无数病患带来无限希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
30
#COMMUN#
40
#新突破#
27
#3D技术#
34
#脑瘤#
34
#3D#
26
学习了
93