JACC:高静息心率与2型糖尿病存在共同的遗传基础
2019-10-27 不详 MedSci原创
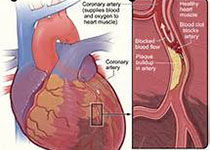
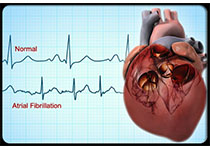
高的静息心率(RHR)常常伴有2型糖尿病(T2D)和代谢综合征,提示可能有共同的发病机制。本研究的目的旨在评估静息心率与心脏代谢疾病/T2D的遗传基础。通过英国生物数据库(n=428250)和其他相关T2D临床试验的数据,本研究发现RHR和T2D有明显的遗传相关性((r = 0.22; 95% cl: 0.18-0.26; p = 1.99 × 10-22),RHR与其他6个心脏代谢特性也存在遗传
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
30
#ACC#
34
#静息心率#
43
谢谢MedSci提供最新的资讯
67
好
77