腰椎融合+PVP术中骨水泥渗漏粘附于下腔静脉滤器1例
2019-04-08 姜平 李念虎 韩瑛光 中国矫形外科杂志
患者,老年女性,68岁,汉族,已婚,45岁绝经。腰痛伴右下肢疼痛麻木7d,10d前患者弯腰抬重物时腰部不慎扭伤,但未出现任何不适感,7d前突发腰痛伴右下肢疼痛麻木,行保守治疗后效果不佳,遂来院就诊。腰痛伴右下肢疼痛麻木,疼痛以右臀部、右大腿后外侧为主,麻木沿右臀部、右大腿前外侧、小腿前外侧至足背、足趾,足趾麻木以第2、3足趾为重,左下肢无任何不适。专科查体:L4棘突及右侧棘突旁压痛,并引起右臀部、
近年来,随着脊柱微创技术的快速发展,经皮穿刺椎体成形术已经成为治疗椎体骨质疏松性压缩骨折(OVCF)的首选方法,但该手术如今仍然存在一些问题,其中最严重、最常见的问题是骨水泥渗漏,一旦发生,可导致严重后果。现报道1例在行腰椎融合+PVP手术时,骨水泥渗漏粘附于下腔静脉滤器的特殊病例,以期对临床工作有所帮助。
经皮穿刺椎体成形术(PVP)是目前治疗骨质疏松性骨折和病理性骨折常用的脊柱微创技术,因其对患者本身创伤小、医疗费用低、疼痛缓解快等优点,在临床上得到了广泛开展与应用。然而PVP也存在一定的风险,尤其是术中注入骨水泥时出现骨水泥的渗漏,其中渗漏到椎体及椎旁静脉血管中因无明显临床症状往往被人们忽视,若发现不及时,会导致肺栓塞、脑栓塞等致命性并发症。为预防骨水泥渗漏,已有许多文献报道采用各种不同技术来降低骨水泥的渗漏风险,如球囊扩张技术(PKP)、编织囊袋技术、改良定向骨水泥推进器、分时间节段灌注、预先填充明胶海绵等,但骨水泥渗漏率仍高达14%。本文通过报道1例行腰椎融合+PVP术中骨水泥渗漏到下腔静脉滤器上的特殊病例,引起广大同道的重视,增强对骨水泥渗漏的预防意识,改进技术,降低骨水泥渗漏风险。
临床资料
患者,老年女性,68岁,汉族,已婚,45岁绝经。腰痛伴右下肢疼痛麻木7d,10d前患者弯腰抬重物时腰部不慎扭伤,但未出现任何不适感,7d前突发腰痛伴右下肢疼痛麻木,行保守治疗后效果不佳,遂来院就诊。腰痛伴右下肢疼痛麻木,疼痛以右臀部、右大腿后外侧为主,麻木沿右臀部、右大腿前外侧、小腿前外侧至足背、足趾,足趾麻木以第2、3足趾为重,左下肢无任何不适。专科查体:L4棘突及右侧棘突旁压痛,并引起右臀部、右大腿后外侧放射性疼痛,右臀部、右大腿前外侧、小腿前外侧、足背、足趾皮肤浅感觉减退,鞍区感觉正常,四肢关键肌肌力正常,右侧直腿抬高试验(+),约60°,余反射及检查正常,病理征未引出。
诊断:(1)L4椎体骨质疏松性压缩骨折(VAS评分9分,压缩率20%);(2)腰椎管狭窄症(L4/5、L5S1,ODI评分68%)。辅助检查:CT见L4/5、L5S1椎间盘向后突出,L4/5椎管变窄,L5S1椎间隙见气体密度影,L5S1椎间盘后缘见斑片状钙化;MRI见L4椎体形态欠规则,椎体边缘欠光整连续,可见长T1信号,压脂像为高信号,L5椎体下缘压脂像可见片状高信号,L4/5、L5S1椎间盘向后方突出,硬膜囊受压,L4/5水平双侧神经根管及L4/5水平椎管受压变窄(图1)。实验室检查结果:血常规+CRP、血沉、住院生化等数值均无明显异常,凝血四项中血浆纤维蛋白原测定和血浆D-二聚体数值均高于正常范围,为排除手术禁忌,行双下肢静脉彩超,结果示:右小腿肌间静脉血栓形成。请周围血管科专家会诊,会诊建议行下腔静脉滤器置入术以保障骨科手术进行。
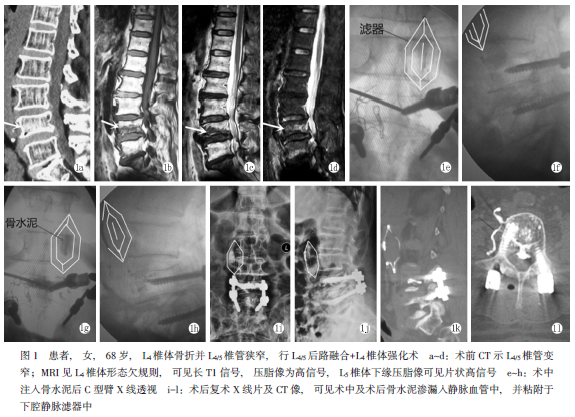
手术方式:患者主要责任节段为L4/5,可行L4椎体PVP+L4/5右侧半椎板切除椎管减压椎间植骨融合内固定术。患者取俯卧位,常规消毒、铺巾。术中C型臂X线机透视定位行左侧L4椎弓根体表投影,0.5%利多卡因局部浸润麻醉后,在X线引导下行L4椎体左侧椎弓根穿刺,调整穿刺针前端置于椎体前中1/3处时,混合搅拌骨水泥,在骨水泥拉丝期通过工作通道缓慢注入伤椎,透视下见骨水泥渗漏,进入椎体前缘静脉丛,沿静脉丛血管进入下腔静脉,并被下腔静脉中的滤器(位置约在最低肾静脉开口下25px)阻挡,骨水泥粘附于滤器上,位置较稳定,患者未出现呼吸困难、憋喘等肺栓塞情况,术中麻醉满意,手术顺利,术后患者安返病房,给予心电监护、持续吸氧,密切观察病情变化。
术后第2d复查腰椎X线片、CT示:L2/3水平右侧脊柱旁可见腔静脉滤器影,内见斑片状致密度影(图1红色标记处)。术后12d,患者病情平稳,腰部疼痛及右下肢疼痛麻木明显减轻,需家人搀扶下地活动,VAS评分5分。患者及家属要求取出滤器,并再次行双下肢静脉彩超,请周围血管科专家会诊,会诊医师详询术后病情并查阅术中及术后影像学资料,分析在骨水泥粘附于滤器的情况下取出滤器的风险较大,建议滤器终生携带,并给予相应的治疗方案,患者及家属权衡利弊,同意会诊专家建议,不再取出滤器,并予以抗凝治疗。
术后随访:术后1个月患者于门诊复查,腰椎X线片示(图1m、n):腰椎内固定无松动迹象,位置良好,粘附于下腔静脉滤器上的骨水泥状态稳定,较出院前腰椎X线片表现无明显变化,患者精神状态良好,未出现胸闷、憋喘等症状,腰痛、右下肢疼痛症状基本缓解,右足2、4趾稍有麻木感,自己佩戴支具可下地行走约100m左右,VAS评分2分,ODI评分40%。术后2个月电话随访,患者精神状态良好,无憋喘、胸闷等症状,自己佩戴支具下地行走约400m左右,日常生活基本可自理,足趾麻木感基本消失,ODI评分约26%。术后半年再次随访,患者无明显不适,已不需佩戴支具可独立行简单的家务劳动,足趾麻木消失,ODI评分约14%。
讨论
随着社会老龄化趋势加剧,老年人日益增多,随之而来的是骨质疏松群体日渐庞大,骨质疏松不仅会引起全身疼痛,更容易造成骨质疏松性压缩骨折(OVCF)。本例患者诊断为骨质疏松性压缩骨折,诊断依据为:(1)患者68岁,45岁绝经,绝经年龄较早,女性患者绝经后体内的雌激素水平急剧下降,破骨细胞的活性增强,从而骨量丢失加速;(2)骨质疏松时,椎体骨组织的减少始于松质骨,逐渐向皮质骨扩展,横向张力性骨小梁最先被累及,严重时在普通X线片上可以显示,第一次在普通X线片上显现大约有30%~80%的骨钙丢失,随着骨质疏松程度的增加,椎体中央与终板相比变得更透光,横向骨小梁广泛丢失和变细,纵向骨小梁明显,皮质逐渐变薄,在影像上表现为纵向层状结构,患者腰椎CT像上栅栏状改变明显;(3)双能X线吸收测定法检测,患者骨密度示:骨质疏松;(4)患者因弯腰搬物品时扭伤腰部导致腰椎骨折,受伤外力小,骨质疏松患者常因较小外力而出现骨折,该患者符合骨质疏松性压缩骨折特点。
骨水泥血管渗漏主要为椎体旁、椎间隙、椎管内、椎体周围静脉渗漏及远隔器官栓塞(肺栓塞、脑栓塞),人体解剖发现正常椎体静脉系统是由骨间、硬膜外和椎旁三套无瓣膜的静脉网所组成,椎体内的小梁间隙包含无数的血管通道,这些通道可来自一根或更多的汇入静脉。骨水泥的渗漏目前常用的是Yeom分型,Yeom等根据骨水泥渗漏的部位将其分为3种类型:B型(椎基底静脉渗漏),骨水泥沿椎基底静脉渗漏到椎体后缘,硬膜的前方,主要局限在硬膜外静脉丛;C型(骨皮质缺损渗漏),骨水泥沿病变椎体骨皮质缺损渗漏,可发生在病变椎体周围的任何位置;S型(节段静脉渗漏),骨水泥沿椎间静脉渗漏,局限在椎间静脉内。通过临床发现及查阅相应文献发现C型骨水泥渗漏的概率较高,笔者认为本文中的病例应属B型+S型,不仅骨水泥渗漏到椎体后缘硬膜的前方而且渗漏到椎旁静脉中并进入到下腔静脉,而骨水泥椎旁静脉渗漏作为渗漏的一种类型,理论上危险性比其他类型渗漏要大,其有可能会引起肺栓塞,因为骨水泥椎旁静脉渗漏不仅局限于静脉内,有时可随血液回心导致肺栓塞,从而产生致命性危险情况,本例患者由于下腔静脉滤器的存在,拦截了渗漏到静脉中的骨水泥,阻挡了骨水泥的继续前行,避免了并发症的出现,因此必须时刻警惕到PVP潜在的危险性,提高警惕,最好术前评估及相应准备。
下腔静脉滤器真的可以预防骨水泥综合征的发生么?2009年第四军医大学师晓琴团队曾行“下腔静脉过滤器对骨水泥置入综合征预防作用”的研究,通过预先在绵羊体内置入滤器,设计对照来观察滤器对骨水泥置入综合征的预防作用,研究结果证实:下腔静脉滤器对骨水泥置入综合征是一种有效的预防措施。下腔静脉滤器作为一种置入物,可能有很多副作用,例如:继发性血栓、滤器脱落、移动等,虽然可以预防骨水泥置入综合征的发生,但也需不断改良,提高质量,减少滤器本身置入后的并发症。通过对此病例的治疗,笔者产生一个有待进一步探讨、研究的想法:在行PVP、PKP等手术时,根据术前影像资料,对于椎体骨折开口较大且椎体壁破损严重,评估骨水泥渗漏风险大的患者术前是否可以预防性置入下腔静脉滤器以防止肺栓塞等发生?具体应用性及价值有待临床进一步研究。
骨水泥渗漏的因素主要与骨水泥灌注时间过早、骨水泥浓度过低、注入压力过大、穿刺针位置等有关,这就要求术前根据影像资料,制定好相应的手术方案,降低骨水泥的渗漏。作者认为降低骨水泥渗漏率需注意以下几点:(1)术前完善CT、三维重建及MR等影像学检查,明确责任椎体,详细了解椎体的损伤情况,如发现骨皮质破损者操作须细致谨慎;(2)忌术中盲目穿刺,要根据C型臂透视影像准确穿刺,切勿凭经验操作,否则必然会增加骨水泥渗漏的风险;(3)有研究表明高黏度骨水泥能有效降低骨水泥渗漏率,术前应充分了解不同厂家骨水泥的特性,选用熟悉的高黏度骨水泥产品;(4)改良传统的骨水泥推注器,形成新型的定向骨水泥推注器,骨水泥推注器的远端为封闭状态,开口呈椭圆形,位于推注器末端的侧方,通过旋转可以控制骨水泥的灌注方向,从而降低渗漏率;(5)术中注意骨水泥注入时间及注入量,对椎体皮质无破损者宜在拉丝早期推注,而椎体皮质有破损者宜在拉丝后期或团状早期推注;(6)骨水泥推注时需注意控制速度,常规每推注0.5ml左右进行一次透视,如发现有m、n:术后1个月X线片示内固定位置良好,无松动渗漏迹象,可减少每次注入量,增加透视次数,一旦发现渗漏存在,并且向椎管内渗漏,即停止渗漏侧骨水泥注入,可改为对侧穿刺或者分时间节段注入,待已注入的骨水泥稍硬化后再继续注入骨水泥;(7)时刻提醒术者骨水泥注入量、骨水泥在椎体内填充百分比与临床止痛效果无直接关系,无须刻意追求尽量多的骨水泥填充,现比较公认的是一般胸椎3ml以内,腰椎5ml以内即可;(8)对于椎体壁破损者,可在注入骨水泥前预先将明胶海绵填充到椎体内,明胶海绵被吸收之前能起到一定的机械屏障作用,直接封堵椎体破口,阻止骨水泥渗出。术后总结本例患者出现骨水泥渗漏原因可能为:(1)L4椎体前缘变扁,椎体前壁存在破坏;(2)L4椎体右侧预先置入椎弓根螺钉,使椎体内压力分布出现变化,在椎体内压力作用下骨水泥渗漏。
综上所述,通过本例病例的处理,加强了对骨水泥渗漏危险性的认识,今后应增强对骨水泥渗漏的预防意识,改进技术,降低骨水泥渗漏风险。
原始出处:
姜平;李念虎;韩瑛光; 腰椎融合+PVP术中骨水泥渗漏粘附于下腔静脉滤器1例报道;《中国矫形外科杂志》2019年第05期
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PVP#
31
#静脉#
43
#下腔静脉#
53
#腔静脉滤器#
31
#腰椎融合#
42
#腰椎#
23
#骨水泥#
43
#融合#
31