EUR J Cancer:基于随机试验的meta分析:贝伐单抗在实体瘤中的作用
2017-12-30 MedSci MedSci原创
贝伐单抗是一种人源化的单克隆抗体,能够抑制循环血管内皮生长因子与其受体的结合。 迄今为止,美国FDA已经批准贝伐单抗用于治疗多种实体瘤。为了评估以贝伐单抗为基础的治疗方案对这些晚期实体瘤患者的影响,研究人员进行了一项meta分析,研究人员对所有的随机试验(II期或III期)中贝伐单抗、安慰剂和其他抗肿瘤药物进行了对比。
贝伐单抗是一种人源化的单克隆抗体,能够抑制循环血管内皮生长因子与其受体的结合。 迄今为止,美国FDA已经批准贝伐单抗用于治疗多种实体瘤。为了评估以贝伐单抗为基础的治疗方案对这些晚期实体瘤患者的影响,研究人员进行了一项meta分析,研究人员对所有的随机试验(II期或III期)中贝伐单抗、安慰剂和其他抗肿瘤药物进行了对比。
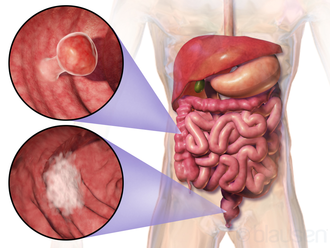
该项以随机对照试验(RCTs)为基础的文献meta分析的主要终点是总生存(OS),次要终点是无进展生存(PFS)时间,有效率和安全性。在结直肠癌,肺癌,卵巢癌和肾癌治疗中,基于贝伐单抗治疗方案显示出了显著提高的总生存期(HR 0.92,95%置信区间[CI]:0.88-0.95;P <0.0001),PFS(HR 0.72,95% CI:0.67-0.78;P <0.00001)和客观反应率(HR 1.38,95% CI:1.27-1.50;P <0.00001)。 但值得注意的是,在乳腺癌中没有观察到对总生存的影响。
因此,这项研究证实了以贝伐单抗为基础的方案对晚期结直肠癌,肺癌,卵巢癌和肾癌的生存期和客观反映率具有显著效果。
原始出处:
Roviello,
Giandomenico, et al. "The role of bevacizumab in solid tumours: A
literature based meta-analysis of randomised trials." European Journal of
Cancer 2017 75: 245-258. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Meta#
24
#MET#
39
#贝伐#
33
#随机试验#
23