Pharmacotherapy:ACS:三种口服抗血小板药物治疗的临床结局
2017-10-12 吴星 环球医学
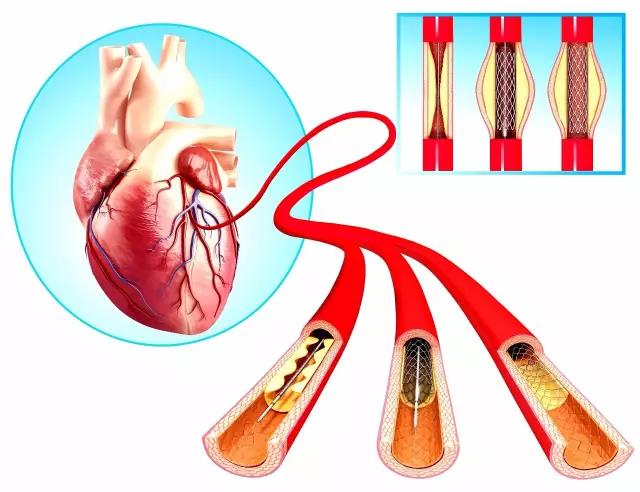
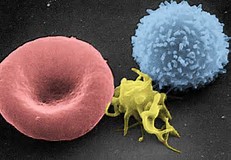
口服抗血小板治疗是急性冠脉综合征(ACS)治疗的基石,随着新型口服抗血小板逐步在临床应用,为依据ACS患者的不同类型进行合理的治疗带来了更多选择。2017年8月,发表在《Pharmacotherapy.》的一项研究比较了ACS患者口服抗血小板药物氯吡格雷、普拉格雷和替格瑞洛的临床结局。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#pharma#
28
#抗血小板药#
41
#ERA#
43
#血小板药物#
45
#Pharm#
29
#临床结局#
32
#MAC#
30
#ACS#
34
henhao
61
学习一下谢谢分享
47