ASCO 2020丨遗憾!早期局部治疗未能改善原发IV期乳腺癌女性的总生存率
2020-06-04 陶然 健康界
早期局部治疗不能提高复发转移性乳腺癌和IPT患者的生存率。虽然在没有LRT的情况下,局部疾病进展的风险高出2.5倍,但IPT的LRT并没有使HRQOL得到改善。
2020年美国临床肿瘤学会(ASCO)年会已经圆满结束,这场学术盛宴可谓精彩纷呈,赢得了全世界肿瘤医生的瞩目。其中最受关注的重磅研究摘要(Late-breaking Abstract,LBA)于美国东部时间5月28日下午5点正式公布,共有2篇入选oral abstract session,5篇LBA入选plenary session。快跟随小编的步伐,开启云年会模式,纵览这些重磅研究吧。
本期和大家分享的是入选plenary session的一篇LBA(摘要号为LBA2),该摘要报告了全身治疗联合早期局部治疗与单独全身治疗对比用于原发IV期乳腺癌女性的随机III期试验。
 图1 ASCO 2020入选的LBA研究(摘要号:LBA2,图源:ASCO 2020官网)
图1 ASCO 2020入选的LBA研究(摘要号:LBA2,图源:ASCO 2020官网)
研究背景
在新诊断的乳腺癌患者中,约有6%的患者有IV期疾病和完整的原发肿瘤(intact primary tumor,IPT)。根据回顾性分析,IPT的局部区域治疗(locoregional treatment,LRT)被假设能提高生存率,但随机试验提供了相互矛盾的数据。我们现在报告E2108的结果,这是一项III期试验,检验了LRT在初始全身治疗后对IPT的价值。
研究方法
对有IPT的IV期患者进行登记,根据患者和肿瘤特点采用最佳系统治疗(optimal systemic therapy,OST)进行治疗;在OST的4~8个月内没有进展的患者被随机分为IPT组的LRT组或无LRT组。
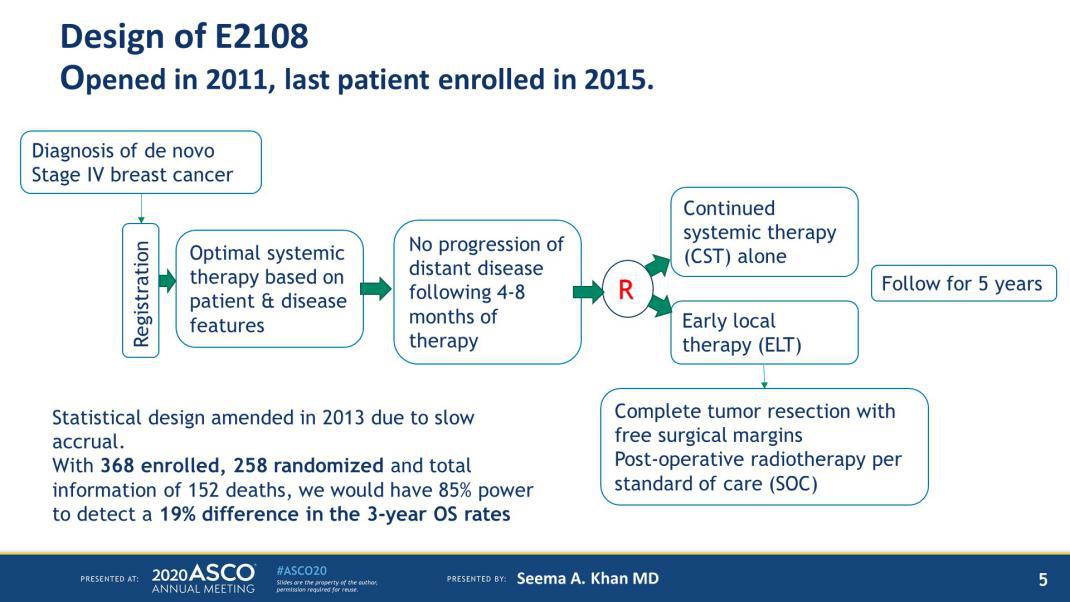 图4 研究设计
图4 研究设计
主要终点为总生存率(OS),局部区域疾病控制为次要终点。采用分层对数秩检验和Cox比例危险模型比较处理组间的OS。估计局部区域复发/进展的累积发生率,并用Gray试验进行治疗组比较。
该试验旨在检测3年OS能否从单纯OST的30%提高到OST+LRT时的49.3%(功率为95%,单侧α 0.05),且152例死亡后有预期的完整信息;数据监测委员会建议有80%的完整信息后再发布数据。
研究结果
从2011年8月2日至2015年7月23日,共有390例患者接受了OST治疗。其中256例符合条件的患者被随机分为单用OST(N=131)或OST+LRT(N=125),中位随访59个月(范围:0~91),共有121例死亡,有43例处于局部进展期。
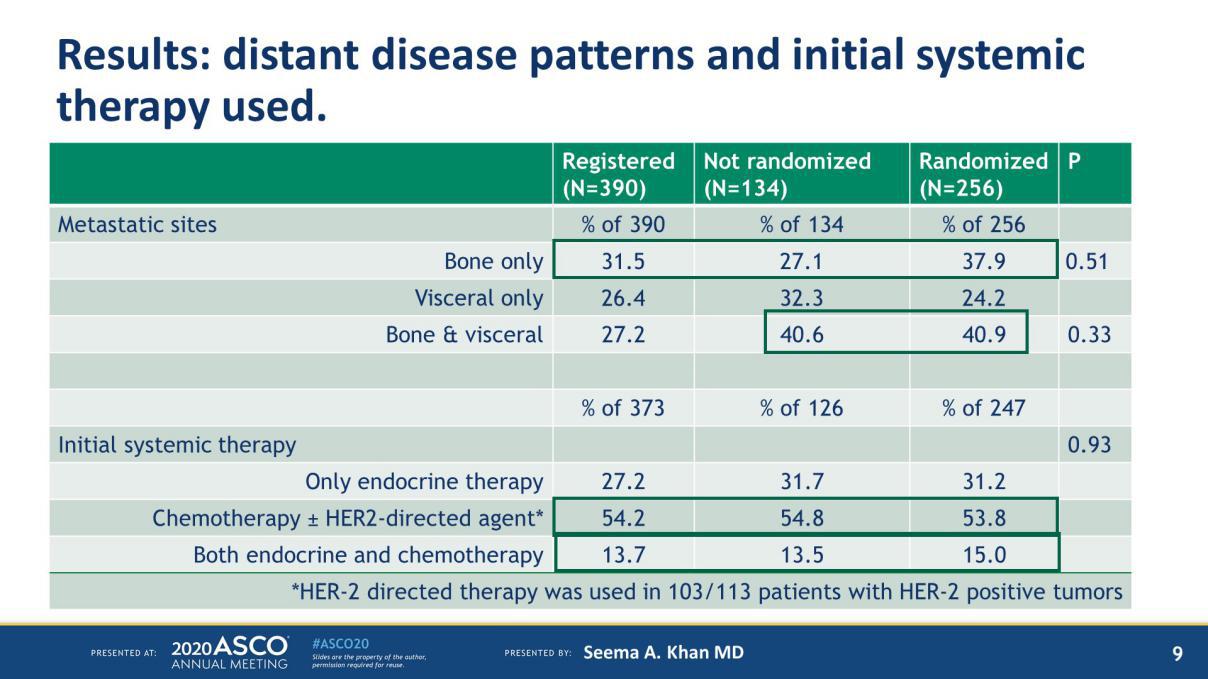 图8 受试者转移位点及最初的全身治疗情况
图8 受试者转移位点及最初的全身治疗情况
OS(OST+LRT组3年OS率为68.4%,单独OST组为67.9%,分层对数秩P=0.63,HR=1.09,90% CI:0.80,1.49)或无进展生存率(P=0.40)无显著性差异。
单用OST组的局部区域复发/进展显著高于对照组(3年复发率为25.6% vs. 10.2%,Gray检验P=0.003)。
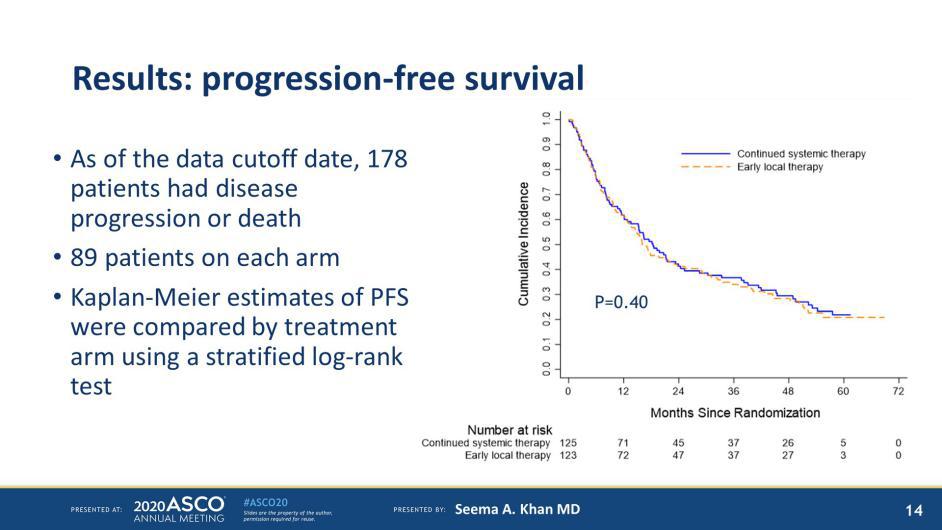 图11 受试者PFS分析
图11 受试者PFS分析
在随机化后18个月(60%完成,Wilcoxon秩和检验P=0.01),由FACT-B试验结果指数测量的OST+LRT组的健康相关生活质量(health-related quality of life,HRQOL)明显低于OST单独组,但在6个月(74%完成)或30个月(56%完成)的时间点没有观察到差异。
结论
早期局部治疗不能提高复发转移性乳腺癌和IPT患者的生存率。虽然在没有LRT的情况下,局部疾病进展的风险高出2.5倍,但IPT的LRT并没有使HRQOL得到改善。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
0
#生存率#
29
#ASCO 2020#
43
#局部#
35
#局部治疗#
47