Hepatology:雄激素受体过度表达与AR-mTOR在肝细胞癌中的意义!
2017-12-12 MedSci MedSci原创
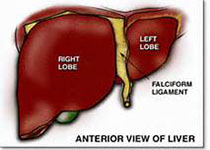
肝细胞癌(HCC)在男性中的发病率较高,这可能由于雄激素受体(AR)与HCC的发病机制有关。然而,AR表达及其在HCC中的确切作用仍然存在争议。此前在HCC中进行的抗雄激素和抗AR的相关临床试验未能显示出其临床益处。近期,一项发表在Hepatology上的研究发现,在大约37%的HCC肿瘤的细胞核中存在AR的过表达,并且,其与晚期疾病阶段和患者的存活不良相关。在HCC细胞中,AR过度表达显着改变A
肝细胞癌(HCC)在男性中的发病率较高,这可能由于雄激素受体(AR)与HCC的发病机制有关。然而,AR表达及其在HCC中的确切作用仍然存在争议。此前在HCC中进行的抗雄激素和抗AR的相关临床试验未能显示出其临床益处。
近期,一项发表在Hepatology上的研究发现,在大约37%的HCC肿瘤的细胞核中存在AR的过表达,并且,其与晚期疾病阶段和患者的存活不良相关。
在HCC细胞中,AR过度表达显着改变AR依赖性转录组,刺激致癌性生长并决定对恩扎鲁胺(enzalutamide,第二代AR拮抗剂)的治疗反应。然而,抑制AR可以引起AKT-mTOR信号的反馈激活,AKT-mTOR信号是细胞生长和存活的中心调节器。另一方面,mTOR通过抑制泛素依赖性AR降解和增强AR核定位来促进核AR的蛋白表达,这就为HCC核中AR过表达提供了相关的解释机制。最后,AR和mTOR的共同靶点显示出显着的协同抗HCC活性,并通过诱导体内细胞凋亡来降低肿瘤负荷。
此项研究结果表明:细胞核内AR的过表达与HCC的进展和预后有关。然而,由于反馈激活AKT-mTOR途径,单独的恩扎鲁胺具有有限的治疗效用。而且,mTOR驱动核AR过度表达。共同靶向针对AR和mTOR是HCC有希望的治疗策略。
原始出处:
Zhang H, Li X, et al. Significance and Mechanism of Androgen Receptor (AR) Overexpression and AR-mTOR Crosstalk in Hepatocellular Carcinoma. Hepatology. 2017 Dec 8. doi: 10.1002/hep.29715.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
40
#肝细胞#
41
#雄激素受体#
27
#EPA#
35
学习了.好文章
0