病例分享:这位老年女性在哭泣后出现呼吸困难、晕厥及肢体活动障碍,什么检查结果使医生们捏了一把冷汗?
2018-03-27 唐颖、高云、李丹 呼吸界
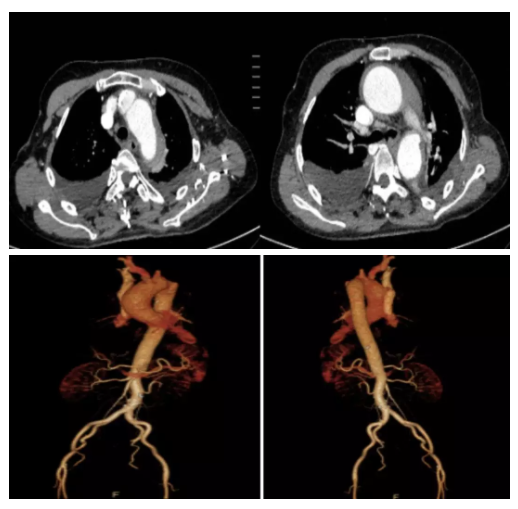
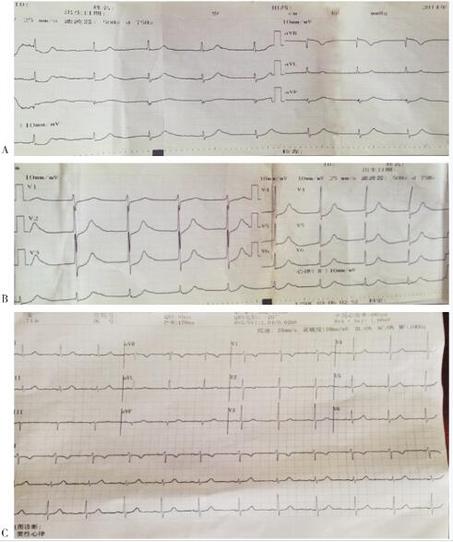
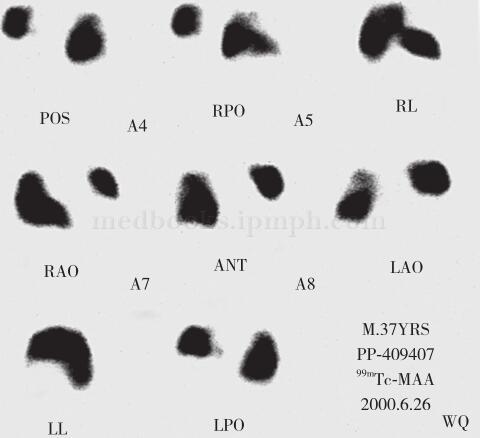
一位老年女性在哭泣后出现晕厥、抽搐、肢体活动障碍,几天后,又陆续出现呼吸困难、咳嗽、休克等症状和情况,在外院就医过程中,经CT检查出了脑梗塞、双侧胸腔积液……
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#检查结果#
37
#活动障碍#
47
学习了
57
#呼吸困难#
38
#晕厥#
36
好病例.谢谢.学习了
53
学习了.谢谢分享.
47