NEJM:临床症状和梗死大小不匹配的卒中:卒中后6到24小时的机械取栓(DAWN)
2017-11-30 贾白雪 首都医科大学附属北京天坛医院
作者:贾白雪 单位: 首都医科大学附属北京天坛医院对于醒后卒中或者发病时间不明确的患者来说,发病时间通常定义为患者最后看起来正常的时间。机械取栓对从最后看起来正常到开始治疗时间超过6小时的患者的有效性仍不明确,尤其是那些存在尚未梗死的可挽救脑组织的患者。这部分患者可以通过与影像显示的梗死体积不匹配的严重症状来识别。在DAWN研究中,研究者对比了血管内机械取栓加
作者:贾白雪 单位: 首都医科大学附属北京天坛医院
对于醒后卒中或者发病时间不明确的患者来说,发病时间通常定义为患者最后看起来正常的时间。机械取栓对从最后看起来正常到开始治疗时间超过6小时的患者的有效性仍不明确,尤其是那些存在尚未梗死的可挽救脑组织的患者。这部分患者可以通过与影像显示的梗死体积不匹配的严重症状来识别。在DAWN研究中,研究者对比了血管内机械取栓加标准药物治疗和单独应用标准药物治疗对于最后看起来正常到治疗的时间6-24小时,并且存在临床症状和梗死体积不匹配患者的有效性和安全性。
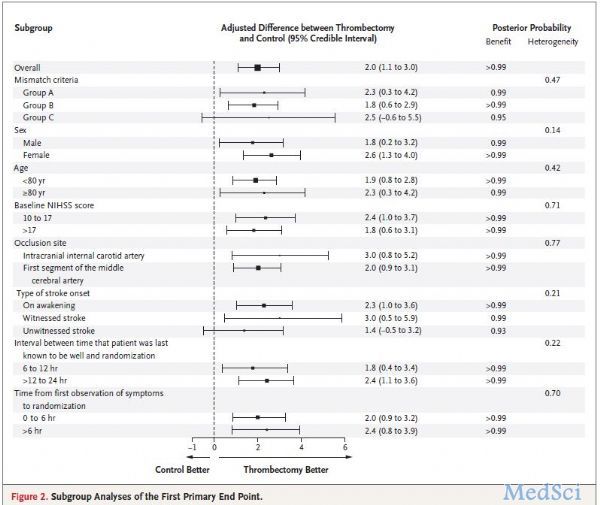
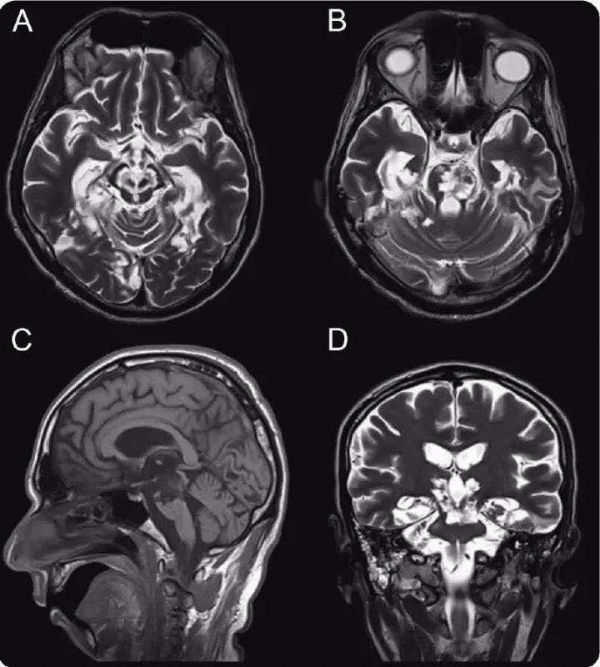
DAWN研究是一项多中心前瞻性随机开放标签结局盲法评价的临床试验。研究在美国、加拿大、欧洲和澳大利亚的26家中心开展,每家中心每年至少开展40例机械取栓。患者的入组标准为:年龄大于等于18岁;最后看起来正常到随机的时间6-24小时;卒中前mRS 0到1分;CTA或MRA证实的颈内动脉颅内段或大脑中动脉M1段或两段同时闭塞;存在临床症状的严重程度与梗死体积不匹配。临床症状的严重程度与梗死体积不匹配的标准为:A组-年龄80岁及以上,NIHSS大于等于10,梗死体积小于21ml;B组-年龄小于80岁,NIHSS大于等于10,梗死体积小于31ml;C组-年龄小于80岁,NIHSS大于等于20,梗死体积31ml到51ml。梗死体积的判断基于磁共振DWI或者CT灌注,采用RAPID软件进行自动计算。
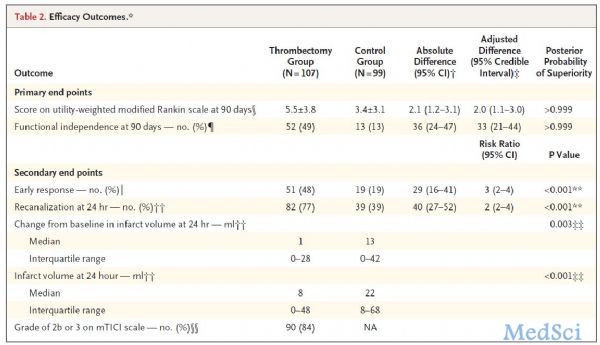
患者按照1:1的比例随机分配到机械取栓加标准内科治疗组(机械取栓组)或单独标准内科治疗组(对照组)。标准内科治疗参照当地的指南。机械取栓应用的是Trevo装置,研究中不允许使用其他装置或药物,术中不允许在颈内动脉颈段植入支架,但必要的时候可以进行颈内动脉颈段的血管成形以通过导管。第一个主要终点事件为90天效用-权重改良Rankin评分的均值。第二个主要终点事件为90天功能独立(mRS0-2分)的比例。次要终点事件有早期治疗反应、90天全因死亡、中心化判读的梗死体积、基线到24小时的梗死体积变化、24小时CTA或MRA显示的闭塞动脉再通。
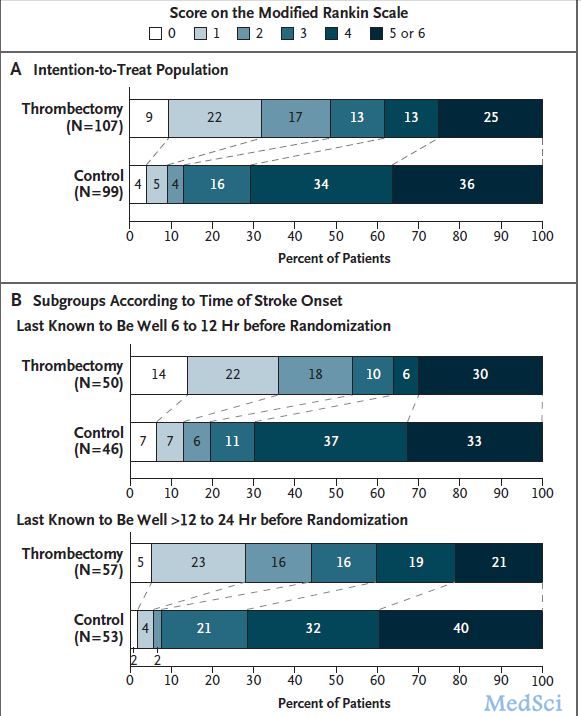
研究共纳入206例患者,其中107例被随机到机械取栓组,99例随机到对照组。两组基线资料基本均衡,NIHSS中位值17,梗死体积中位值分别为7.6ml和8.9ml,最后看起来正常到随机的时间分别为12.2和13.3小时。机械取栓组患者术中再通率为84%,24小时再通率两组分别为77%和36%。90天时,机械取栓组的效用-加权mRS优于对照组(5.5vs3.4,调整后差异2.0分,95%CI 1.1-3.0),90天功能独立的比例同样也显示出机械取栓的优势(49%vs13%,调整后绝对差33%,95%CI 24-44%)通过事后敏感性分析调整了组间基线资料差别以后,机械取栓的优势仍然是显著的。所有的次要终点事件的比较,机械取栓组均优于对照组。
本研究机械取栓组功能独立的比例与五大研究汇总分析的结果相似(分别为49%和46%),而对照组则较五大研究汇总分析的对照组低(13%和26%)。可能的原因有,本研究对照组静脉溶栓比例更低、高龄患者更多、卒中严重程度更重。
研究者认为对于从最后看起来正常到治疗时间6-24小时的颈内动脉颅内段或大脑中动脉近段闭塞引起的急性缺血性卒中患者,如果同时存在临床症状严重程度和梗死体积不匹配,则接受机械取栓加药物治疗比单纯药物治疗90天的功能独立更好。
作者点评:
DAWN研究为急性缺血性卒中血管内治疗时间窗的延长提供了新的证据,可能使更多的患者从机械取栓术中获益,这是值得兴奋的。与此同时,我们应注意研究中的两个关键点。第一,文中反复提及的时间窗概念是从“最后看起来正常的时间”开始计算,即使在标题中(有字数限制),也谨慎地用了“卒中后6-24小时”而非“发病后6-24小时”。事实上,本研究中85%-90%的患者是醒后卒中或者发病时间不明确的卒中,这部分患者实际的发病到治疗时间很可能是小于这个时间窗的。对于发病时间明确的患者,不应简单粗暴地套用6-24小时的时间窗。第二,研究严格把握了临床症状和梗死体积不匹配这一标准,两组NIHSS评分中位值在17分,而梗死体积的中位值在两组均小于10ml(分别为7.6ml和8.9ml),因此,术前采用MRI的DWI或CTP进行梗死体积的严格评估也是非常必要的。总之,DAWN研究给我们带来了新的希望,但一个临床研究的价值远不是得出一个简单的结论,仔细研读全文有助于临床医生更客观和准确地解读研究结果。
参考文献
Nogueira RG, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. New Engl J Med 2017; DOI:10.1056/NEJMoa1706442.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#24小时#
44
#临床症状#
49
#卒中后#
42
学习了.谢谢分享!
77
#取栓#
34
#机械取栓#
37
学习了.好文章
74