Circulation:Ross手术可替代机械主动脉瓣置换术(AVR)
2016-08-23 fsy 译 MedSci原创
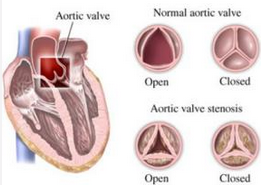
在年轻人和中年人中,理想的主动脉瓣替代疗法仍然不明。研究人员试图比较接受Ross手术和接受机械主动脉瓣置换术(AVR)患者的长期结果。从1990年到2014年,在一个单一机构中,258例患者接受了Ross手术,1444例患者接受了机械AVR。研究人员通过使用倾向得分将患者匹配分成208对。这些患者的平均年龄为37.2±10.2岁,63%为男性。平均随访时间为14.2±6.5年。虽然Ross组的无心
在年轻人和中年人中,理想的主动脉瓣替代疗法仍然不明。研究人员试图比较接受Ross手术和接受机械主动脉瓣置换术(AVR)患者的长期结果。
从1990年到2014年,在一个单一机构中,258例患者接受了Ross手术,1444例患者接受了机械AVR。研究人员通过使用倾向得分将患者匹配分成208对。这些患者的平均年龄为37.2±10.2岁,63%为男性。平均随访时间为14.2±6.5年。
虽然Ross组的无心脏和瓣膜相关的死亡率明显改善(Ross vs AVR:危险比,0.22;95%置信区间,0.034-0.86;P=0.03),但两组患者的总生存率是一样的(Ross vs AVR:危险比0.91,95%置信区间,0.38-2.16; P=0.83)。两组患者经过手术后无再次干预的概率也是一样的(Ross vs AVR:危险比,1.86; 95%置信区间,0.76-4.94; P=0.18)。 Ross组患者手术后无卒中或大出血的长期结果要优于AVR组(Ross vs AVR:危险比, 0.09;95%置信区间,0.02-0.31; P<0.001)。
在Ross手术组和机械AVR组之间,长期的生存和无再次干预治疗的结果是一样的。然而,Ross手术组的无心脏和瓣膜相关死亡都有所改善,并且卒中和大出血的发生率都显著减少。在专业的治疗中心中,Ross手术是一个很好的选择,所以接受AVR的年轻人和中年人可以考虑接受Ross手术。
原始出处:
Amine Mazine, Tirone E. David, Vivek Rao,et al.Long-Term Outcomes of the Ross Procedure Versus Mechanical Aortic Valve Replacement,Circulation,2016.8.23
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AVR#
35
#置换#
31
在学习了
49
文章很好值得关注
55
#Ross手术#
31
越来越先进发达。
1
很好的文章,读一读有好处。
55
学习了,赞一个!!
58
学习了,赞一个!!
25
谢谢,学习了。
28