下颌第二磨牙远中骨缺损致牙周牙髓联合病变1例
2019-02-15 王桂红 牙体牙髓牙周病学杂志
患者男,30岁。2015-10因右下颌磨牙区肿痛前来就诊,3个月前曾行48拔除术。检查:张口正常,47无龋损,远中颊侧牙龈红肿,触痛,远中PD15mm、CAL13mm,松动Ⅱ°,叩(++),牙髓活力(-)。X线片示:47远中至根尖处可见稀疏区。诊断:47远中骨缺损,牙周牙髓联合病变。治疗计划:47行根管治疗术;远中行植骨术+GTR;择期冠修复。
下颌第三磨牙近中阻生时,常因食物嵌塞、阻生第三磨牙拔除后致第二磨牙远中骨缺损。阻生第三磨牙拔牙创愈合后,第二磨牙远中仍有不同程度的牙槽骨吸收,容易继发龋损、牙齿松动、牙周病变等。
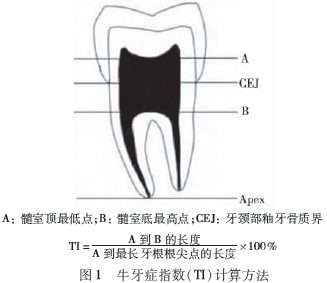
第二磨牙经牙周治疗和单纯性生物膜覆盖后,其基骨再生效果也不显著。引导组织再生术(GTR)是在牙周手术中利用生物膜材料作为屏障,阻挡牙龈上皮和牙龈结缔组织在愈合过程中向根面生长,进而引导具有形成附着能力的牙周膜细胞优先向根面生长,从而在病变根面上形成新的牙骨质并有牙周膜纤维埋入,形成新附着性愈合。本文报道1例用植骨术+GTR治疗下颌第二磨牙远中骨缺损致牙周牙髓联合病变患者。
1.病例报告
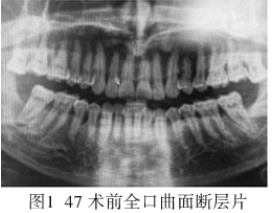
患者男,30岁。2015-10因右下颌磨牙区肿痛前来就诊,3个月前曾行48拔除术。检查:张口正常,47无龋损,远中颊侧牙龈红肿,触痛,远中PD15mm、CAL13mm,松动Ⅱ°,叩(++),牙髓活力(-)。X线片示:47远中至根尖处可见稀疏区。诊断:47远中骨缺损,牙周牙髓联合病变。治疗计划:47行根管治疗术;远中行植骨术+GTR;择期冠修复。
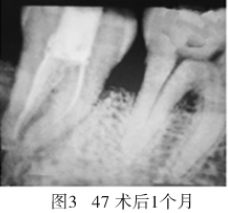
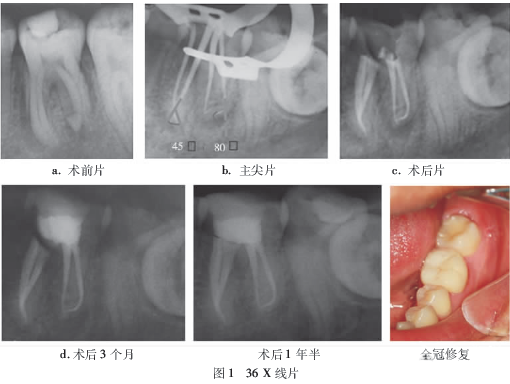
治疗:47开放引流,远中牙周袋内冲洗上药,口服抗生素3d。3d后复诊,47叩(-),松动Ⅱ°,常规根管治疗术。局麻下行47远中植骨术+GTR:翻瓣,暴露颊侧及远中骨面,见远中骨缺损至根尖,宽约3mm;刮净肉芽组织,生理盐水冲洗术腔,植入Bio-Oss骨粉后,覆盖胶原膜并严密缝合切口,术后口服抗生素,1周后拆线。术后1个月复诊,47叩(-),无松动,PD3mm;行冠修复。术后1.5年复诊,47叩(-),远中骨密度较正常骨质稍低(图1~4)。


2.讨论
下颌第三磨牙近中阻生拔出后,易导致下颌第二磨牙远中骨缺损、远中龋损、牙周病等。本病例提示,在拔除阻生第三磨牙时,应尽可能保留下颌第二磨牙远中骨质,少去骨,特别是保留远中颊侧骨基点高度。有学者探讨了在拔牙中应用多种方法来避免邻牙远中骨缺损(如下颌第二磨牙远中局部植骨等),均有一定的效果。对于下颌第二磨牙出现远中骨缺损致牙周牙髓联合病变患者,采用植骨术+GTR能取得较好的治疗效果。
本病例中,47在进行根管治疗的基础上,行远中骨缺损处肉芽组织刮除术,同时植入Bio-Oss骨粉,并覆盖胶原膜,这样更有利于远中骨形成及牙周病变的恢复,从而保留患牙。Bio-Oss骨粉为异种骨,具有骨引导作用,无成骨和骨诱导作用;所形成的基质支架有利于邻近组织中的细胞进入植骨材料,从而形成新骨;植骨上面覆盖胶原膜,可防止胶原膜的塌陷,有利于加快远中骨缺损的修复。本例患者现已随访1.5年,患牙无松动及叩痛,能正常咬合。
原始出处:
王桂红.下颌第二磨牙远中骨缺损致牙周牙髓联合病变1例[J].牙体牙髓牙周病学杂志,2018(02):124.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#下颌#
25
#牙髓#
31
#骨缺损#
40
#牙周#
37
#磨牙#
31