全腹腔镜右肾及肾静脉瘤栓切除术 术中术后注意事项需谨记!
2017-10-19 那彦群 陈山 泌尿外科疑难病例讨论精选
26岁女性,半个月前B超体检时偶然发现右肾实性占位病变,无任何临床表现。就医后经诊断为侵袭性肾血管平滑肌脂肪瘤,需要手术治疗。手术方式如何选择?关键步骤的注意事项有哪些?术后注意事项有哪些?
【病例资料】
患者女性,26岁。
主诉:体检发现右肾占位半个月。
现病史:半个月前患者B超体检时偶然发现右肾实性占位病变,无任何临床表现。
【体格检查】
临床查体无阳性体征。
【辅助检查】
实验室检查:血、尿常规及血生化检查未见异常。
影像学检查:
正、侧位胸片和全身骨扫描检查无异常。
B超:右肾窦内可见5.1cm×2.7cm高回声占位,边界欠规则,内见血流信号。
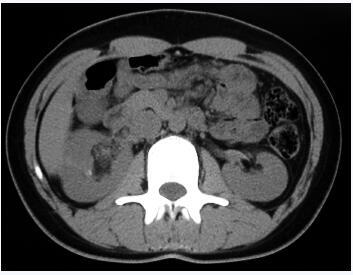
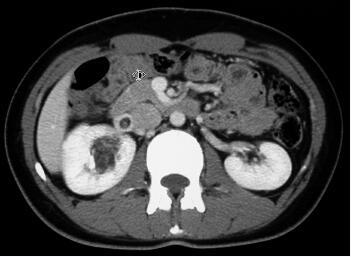
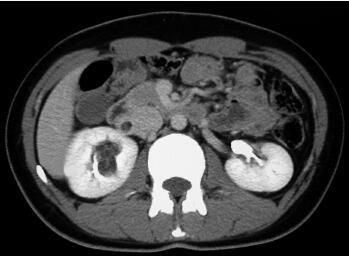
CT平扫:右肾盂旁可见一个不规则团块状混杂密度影,大小4.5cm×2.9cm×1.9cm,最低密度CT值为-40HU。增强扫描病变组织部分明显强化,最高CT值达97HU。增强后显示病变主要位于肾窦,并紧贴肾血管走行,一部分病变组织延伸至肾静脉内,一部分病灶压迫肾盂并与肾实质分界不清,右肾上、中盏受压变形(图18-1~图18-4为该肿瘤的部分CT扫描图像)。

【术前诊断】
肾血管平滑肌脂肪瘤伴肾静脉瘤栓(右)
【治疗经过】
全腹腔镜右肾及肾静脉瘤栓切除术。
术中所见:
1. 麻醉方法及手术路径
采用全麻醉及经后腹腔手术路径。后腹腔制备采用手指扩张法,分别于腋中线髂嵴上2cm、腋前线及腋后线肋缘下、腋前线髂棘上水平置入套管针(trocar)。
2. 手术器械要求
①腋中线髂嵴上2cm处和(或)腋后线肋缘下处需置入的trocar直径须为12mm,以便由此处将腔镜血管夹放入手术位置;②腔镜血管夹阻断血管的宽度除>2cm(可完整阻断肾静脉)外,须有一定的弧度(深度>0.5cm,以便能部分阻断下腔静脉)。
3. 术中重点步骤
①自肾下极沿下腔静脉解剖出肾动脉,Hem-o-lock夹闭肾动脉并切断;②解剖下腔静脉和肾静脉,将腔镜血管夹沿下腔静脉走行,于肾静脉入下腔静脉处部分阻断下腔静脉、完整阻断肾静脉;③于近肾静脉处切开下腔静脉,完整切除肾静脉及肾静脉内瘤栓;④用4-0无创血管吻合线缝合下腔静脉切口,开放血管夹后缝合处无漏血。⑤游离肾脏及输尿管,并完整切除右肾。
【术后诊断】
病理检查结果:肾血管平滑肌脂肪瘤,伴瘤栓形成,部分肿瘤细胞呈上皮细胞样改变。
【术后诊疗】
1. 患者术后1周痊愈出院,术后随访6个月余,未发现肿瘤复发和转移。
2. 术后未予患者任何辅助治疗。
3. 我们建议患者按照肾癌患者的术后要求进行复查,即每半年行腹部超声或CT检查,同时行正、侧位胸片或CT检查;每1年行全身骨扫描检查。
【讨论内容】
文献综述:
肾血管平滑肌脂肪瘤(angiomyolipoma,AML)是来源于肾间质的肿瘤,占肾肿瘤的2%~6.4%,成分包括平滑肌、血管和成熟脂肪。肾AML可为散发,也可为结节性硬化症(tuberous sclerosis complex,TSC)的一部分。20%的肾AML患者患有TSC,而TSC患者中40%~80%伴发肾AML,表现为双肾多灶性AML。
肾AML多为良性肿瘤,但极少部分肾AML表现为侵袭性,甚至为恶性肿瘤。肾AML可侵及肾静脉、下腔静脉及心房等。另外,肾AML的一个特殊亚型肾上皮样AML,目前被认为是一种具有侵袭性生物学行为的恶性肿瘤,可表现为侵袭性生长方式,可侵犯肾静脉、下腔静脉及心房,肿瘤可出现转移和复发,文献报道10余例上皮样AML发生肿瘤转移。因此肾AML并非都是良性肿瘤,少数可为恶性或恶性潜能。
典型肾血管肌脂瘤(AML)超声表现为高回声占位,CT可发现脂肪负值信号。肾上皮样AML在影像学上常易与肾癌、肉瘤样癌混淆,目前尚未见到肾上皮样AML中有脂肪影像的报道。但肾上皮样AML可与肾AML同时发生,也可发生于肾AML内,CT表现为脂肪密度影内可强化的结节。曾有报道典型肾AML伴有核异型上皮细胞者发生肺、肝等远处转移。因此对于有侵袭性生物学行为的肾AML应除外有无伴有或恶变为肾上皮样AML的可能。文献报道近20例典型肾AML侵及肾静脉、下腔静脉及心房等,其中多数为女性患者。更为罕见的病例,一例TSC患者双侧肾AML瘤栓均突入腔静脉内。
【专家点评】
诊断问题:本例患者为肾AML伴有部分上皮细胞样改变,临床表现侵袭性生物学行为。
1. 本病例影像学检查特点B超提示为右肾直径5cm的高回声占位,边界欠规则,内见血流信号;CT平扫见右肾占位为不规则混杂密度影,最低密度
T值为-40HU。增强扫描病变组织部分明显强化,最高CT值达97HU。增强显示病变主要位于肾窦,并紧贴肾血管走行,一部分病变组织延伸至肾静脉内。
2. 鉴别诊断难点 肾AML并肾静脉和(或)下腔静脉瘤栓临床罕见,易误诊为肾细胞癌或其他肾脏恶性肿瘤。
治疗问题:
1. 手术方式的选择 肾AML如果体积较大(肿瘤直径>5cm)、伴有疼痛、出血或怀疑恶变时应进行外科干预,一部分肾AML需行肾切除,多数的肾AML可以保留肾脏(实施肾部分切除术)。以往,对于伴有静脉瘤栓的肾肿瘤多采用开放手术。随着腹腔镜手术技术的不断提高,腹腔镜肾切除的手术适应证也在不断扩大,目前已有人尝试对于伴有肾静脉或下腔静脉瘤栓的肾癌患者行腹腔镜肾切除同时行静脉取栓。文献报道的肾AML伴瘤栓者均采用开放手术,而文献报道肾癌伴有肾静脉或腔静脉癌栓者可经腹腔镜或手助腹腔镜下完成,手助腹腔镜静脉取栓的优势在于可更好的控制大血管出血,及时中转开腹,腹腔镜入路可经腹腔或经后腹腔。
我们为本例患者实施了全腹腔镜右肾及肾静脉瘤栓切除术,其优点是解剖清晰、微创、患者术后恢复快速。
2. 关键步骤的注意事项 腹腔镜取栓术的关键是如何正确放置腔镜血管夹,首先术前应行CT血管重建、MRI或血管造影判断瘤栓突入肾静脉或腔静脉内的深度,也可在术中进一步行超声判断瘤栓边缘。血管夹放置不正确将直接影响腹腔镜取栓的成败。Kapoor等报道12例患者中2例因血管阻断钳放置位置不合适而改行开放手术。其次,血管夹放置需要大通道,一般需要12mm或以上套管针(trocar)。对于仅限于肾静脉内或突入腔静脉内不超过1cm者,因血管阻断钳有一定弧度,一个血管夹即可阻断局部腔静脉,但对于突入腔静脉内超过cm者应在瘤栓上下各放置一个血管阻断钳。最后,在取瘤栓时最好边切开肾静脉或腔静脉,逐步取出瘤栓时边缝合血管,以更好的保证手术的安全性以及瘤栓取出的完整性。
术中也应避免反复调整血管阻夹的位置以防止瘤栓被夹断脱落,如术中瘤栓取出不完整或术中冰冻切缘阳性,应及时转为开放手术。Martin等报道14例患者中1例因术中冰冻切缘阳性而改行开放手术。我们认为对于选择性病例如肿瘤瘤栓局限于肾静脉内或突入腔静脉内较少者行腹腔镜肾切除,同时行肾静脉或腔静脉取栓术安全可行。
术后注意事项:本例患者术前检查虽无肿瘤转移的临床证据,但影像学检查提示肿瘤有侵袭性生物学行为,且术后病理证实为肾AML伴有部分上皮细胞样改变,因此对该患者术后应密切随访,以便观察其有无肿瘤复发和转移。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
31
#静脉瘤#
32
#注意事项#
24
#静脉#
36
#腹腔镜#
25