ATVB:颈动脉斑块钙化与斑块内出血相关!
2017-04-29 xing.T MedSci原创
由此可见,颈动脉粥样硬化斑块表面钙化和多个钙化与IPH存在独立相关,提示钙化数量和位置都可能在IPH的发生中起着重要的作用。这些发现可能为理解IPH的机制提供了新的见解。
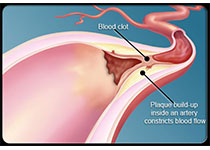
颈动脉斑块内出血(IPH)与心血管事件相关。斑块钙化,经常伴随着IPH,可能在IPH的发生中起了一定的作用。近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,在这项研究中,研究人员旨在探讨钙化特征与颈动脉斑块IPH之间的相关性。
117例脑血管症状和超声检测有颈动脉斑块的患者被招募入研究,并且进行了增强磁共振成像检查。通过磁共振成像测量的进一步颈动脉斑块组成被纳入分析,颈动脉钙化被分为以下几类:表面钙化、混合钙化和深部钙化。同时根据钙化数量,这些患者被分为单个和多个钙化。采用广义估计方程的Logistic回归模型被用来评价钙化与IPH之间的相关性。
在117名受试者中,有85名受试者共计142处斑块被纳入最后的分析,其中32名受试者因为缺乏斑块组成数据而被排除在外。在这142个斑块中,40个(28.2%)斑块存在IPH。存在IPH的斑块比没有IPH的斑块具有更高的钙化发生率(87.5% vs. 55.9%;P=0.005)。在调整了年龄、低密度脂蛋白、最大管壁厚度、最大软斑块厚度后,研究人员发现多发钙化(比值比为10.1;95%可信区间为3.3-30.4)、表面钙化(比值比为29.4;95%可信区间为4.1-210.8)和混合性钙化(比值比为27.9;95%可信区间为7.3-107.1)与IPH的存在密切相关(所有P<0.05)。
由此可见,颈动脉粥样硬化斑块表面钙化和多个钙化与IPH存在独立相关,提示钙化数量和位置都可能在IPH的发生中起着重要的作用。这些发现可能为理解IPH的机制提供了新的见解。
原始出处:
Ruolan Lin,et al. Association Between Carotid Atherosclerotic Plaque Calcification and Intraplaque Hemorrhage A Magnetic Resonance Imaging Study.ATVB.2017. https://doi.org/10.1161/ATVBAHA.116.308360
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TVB#
24
#颈动脉#
25
好文章学习并分享!!
43
学习一下知识,进步
56
#颈动脉斑块#
27
#斑块#
31
#斑块内出血#
41
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦……
47
钙化之后变硬而容易出血
66
学习了谢谢分享
68