Lancet oncol:瑞戈非尼可提高复发性胶质母细胞瘤患者总体存活率(REGOMA研究)
2018-12-08 MedSci MedSci原创
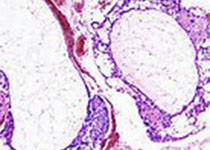
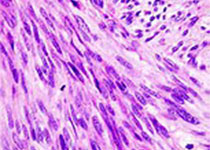
胶质母细胞瘤是一种高度血管化的肿瘤,复发后几乎没有治疗方法。瑞戈非尼是一种口服的血管生成、基质和致瘤受体酪氨酸激酶的多激酶抑制剂。现研究人员对瑞戈非尼用于复发性胶质母细胞瘤的疗效和安全性进行评估。研究人员在意大利的10个中心开展一随机的开放的II期试验,招募年满18岁的组织学确诊的胶质母细胞瘤患者,且要求ECOG表现状态0或1分、手术加上放化疗(替莫唑胺)后病程进展。受试患者被随机(1:1)分至瑞
研究人员在意大利的10个中心开展一随机的开放的II期试验,招募年满18岁的组织学确诊的胶质母细胞瘤患者,且要求ECOG表现状态0或1分、手术加上放化疗(替莫唑胺)后病程进展。受试患者被随机(1:1)分至瑞戈非尼组(瑞戈非尼160mg/日,连用3周,4周一疗程)或洛莫司汀组(110mg/m2·6周),用药至病程进展、死亡、不可耐受的毒性或自主撤出。主要结点是总体存活率。
2015年11月27日-2017年2月23日,共招募到119位符合要求的患者,随机分至瑞戈非尼组(59人)和洛莫司汀组(60人)。中位随访15.4个月(IQR 13.8-18.1)。截止分析日期,99位患者死亡:瑞戈非尼组42位(71%)、洛莫司汀组57位(95%)。与洛莫司汀组相比,瑞戈非尼组的总体存活期显着延长,瑞戈非尼组和洛莫司汀组的中位总体存活期分别是7.4个月(95% CI 5.8-12.0)和5.6个月(4.7-7.3;风险比0.50,95% CI 0.33-0.75,p=0.0009)。瑞戈非尼组和洛莫司汀组3-4级治疗相关副反应的发生率分别为56%和40%。与瑞戈非尼相关的最常见的3-4级副反应是手足皮肤反应、脂肪酶升高和血胆红素升高(均为10%)。洛莫司汀组最常见的3-4级副反应是血小板计数减少(13%)、淋巴细胞计数减少(13%)和中性粒细胞减少(12%)。无药物相关死亡。
本研究显示,瑞戈非尼治疗复发性胶质母细胞瘤可提高患者的总体存活效益,应进行3期临床试验探究瑞戈非尼在胶质母细胞瘤中的治疗潜能。
Giuseppe Lombardi,et al.Regorafenib compared with lomustine in patients with relapsed glioblastoma (REGOMA): a multicentre, open-label, randomised, controlled, phase 2 trial.The Lacnet Oncology. December 03,2018.https://doi.org/10.1016/S1470-2045(18)30675-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胶质母细胞#
45
#母细胞瘤#
37
#Lancet#
0
#复发性#
48
#Oncol#
48
#存活率#
40
#细胞瘤#
51
#复发性胶质母细胞瘤#
48
学习了
80