脾脏硬化性血管瘤样结节性转化超声表现1例
2019-11-12 余锴 梅云华 临床超声医学杂志
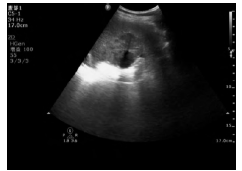
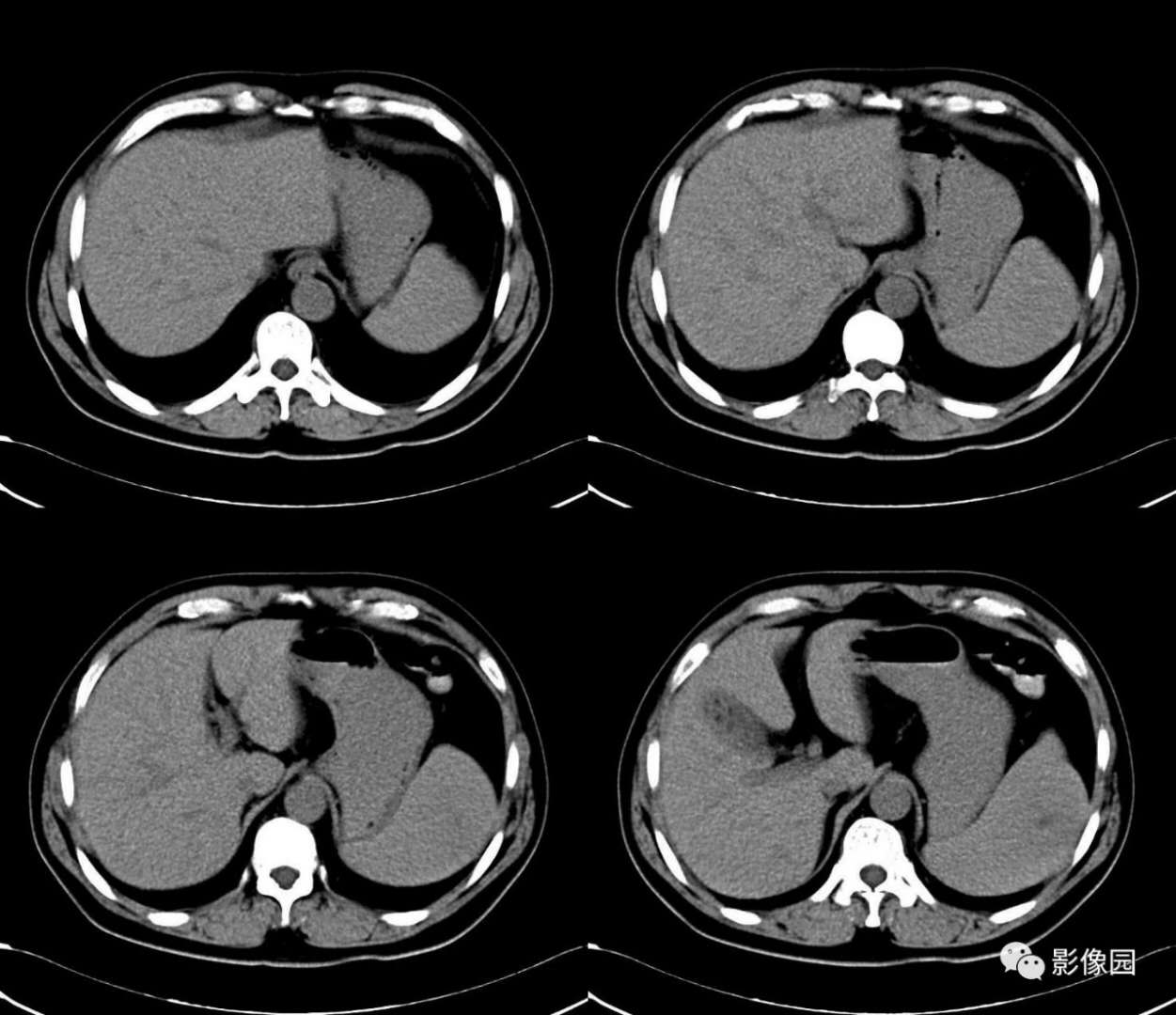
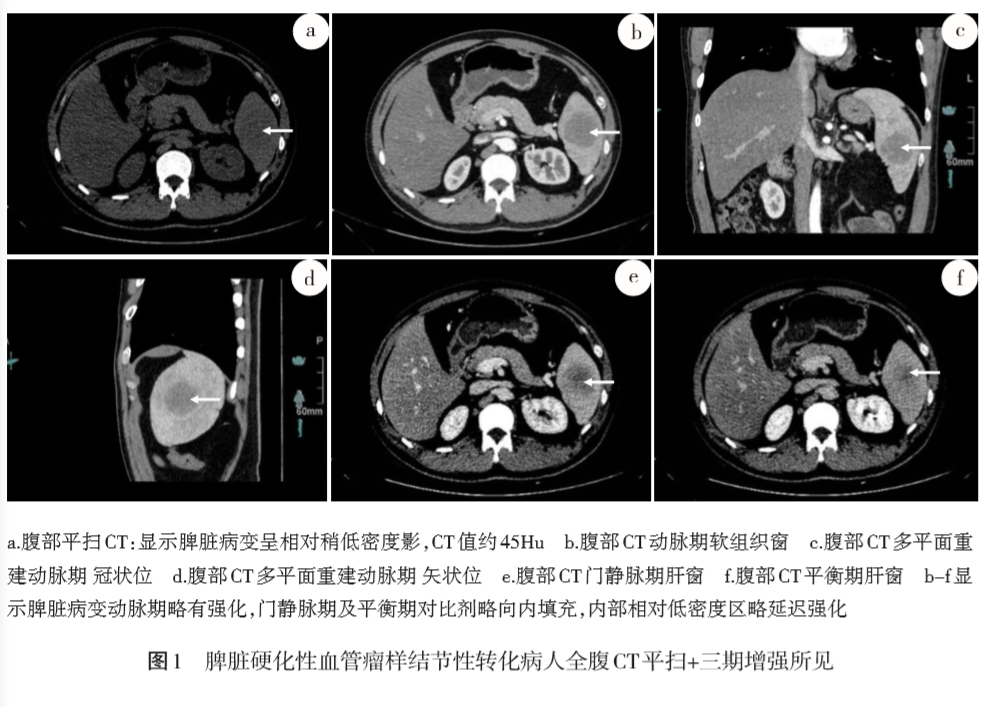
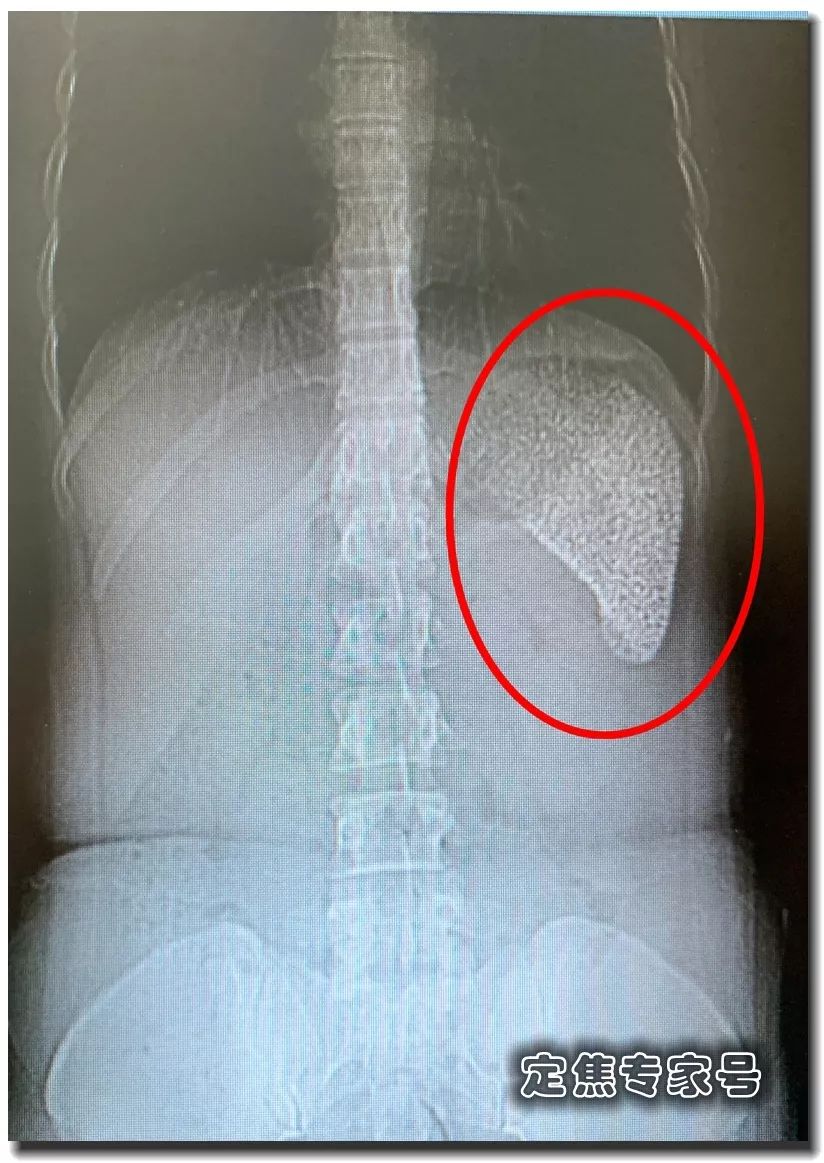
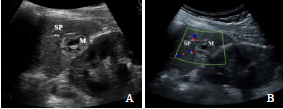
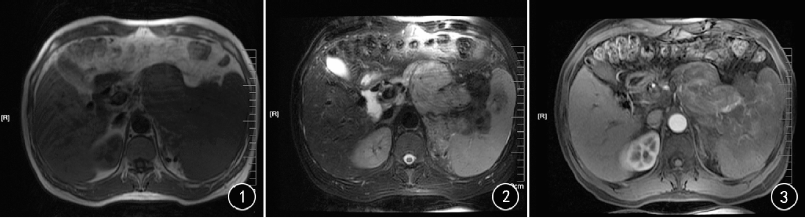
患者女,27岁,因体检发现脾门区肿瘤入院。超声检查:脾脏切面形态失常,实质点状强回声分布不均匀,脾门区可见一个大小为5.2 cm×4.3 cm×4.7 cm的团状低回声向脾脏内凸起,边界欠清晰,内回声不均匀,可见高回声条索样分隔,呈“分叶状”改变。脾门区脾静脉受压迫(图1);CDFI示上述肿块内可见血流信号,周边可见多条血管由肿块表面直插入肿块中心,呈“轮辐状”(图2)。超声提示:脾门区实质性占位

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








见到过
42
#结节性#
29
#超声表现#
37
非常受益,很好的研究
81
非常受益,很好的研究
80
#血管瘤#
38
#硬化性#
28