Arthritis Care Res:RA患者启动或换用DMARD治疗的患者报告结局检测信息系统(PROMIS)反应性
2018-07-11 MedSci MedSci原创
患者报告结局检测信息系统(PROMIS)用于评估患者的多个领域报告结局。Wohlfahrt A等研究者于2018年6月在Arthritis Care Res (Hoboken)上发表了一项在研前瞻性、观察性研究,旨在评估筛选的PROMES指标在评估病情缓解抗风湿病药物(DMARD)治疗活动性风湿性关节炎(RA)患者中的作用。 类风湿关节炎(RA)是一种慢性疾病,若未进行积极管理,可显著影响患者的
患者报告结局检测信息系统(PROMIS)用于评估患者的多个领域报告结局。Wohlfahrt A等研究者于2018年6月在Arthritis Care Res (Hoboken)上发表了一项在研前瞻性、观察性研究,旨在评估筛选的PROMES指标在评估病情缓解抗风湿病药物(DMARD)治疗活动性风湿性关节炎(RA)患者中的作用。
类风湿关节炎(RA)是一种慢性疾病,若未进行积极管理,可显著影响患者的日常生活。医师在评估疾病活动时往往非常依赖于肿胀关节的评估、血液炎症标志物的检测以及放射影像学检测。然而,如果没有患者的直接反馈,医师就无法充分了解疾病活动度及其影响。RA的症状,如疼痛和疲劳,必然需要通过患者的自我报告进行评估。此外,包括患者躯体功能在内的其他因素,通常也需要通过患者报告进行评估。
患者报告结果(PRO)的重要性已在多个领域获得认可——临床试验、临床护理和保险授权。美国风湿病学会(ACR)和欧洲抗风湿病联盟(EULAR)推荐在所有临床试验中采用包括患者总体评估在内的综合指标[例如,临床疾病活动度指数(CDAI)、28个关节疾病活动度评分(DAS-28)和简化疾病活动度指数(SDAI)]报告疾病活动度结果。此外,风湿病结局评估(OMERACT)小组正在针对临床试验中额外PRO的评估制定相关指南。对于RA治疗而言,国际工作组推荐医师应基于疾病活动度综合指标评估患者治疗达标情况,并在制定治疗策略时纳入患者的观点。保险公司也推动医师采用以患者为中心的管理策略,归因于良好的结局在某种程度上被定义为患者的“增值”。内科医师可通过PRO来识别哪些患者可从中获益。虽然PRO的价值已获得广泛认可,但研究者和临床医师常常面临着如何决定使用哪种方法的难题。该项研究重点关注于一种PRO评估工具,即PROMIS。PROMIS开发了一套标准化的评估工具,使得跨疾病比较以及从研究至临床的转化成为可能。并采用固定项简短量表或通过计算机自适应测验(CAT)进行评估。
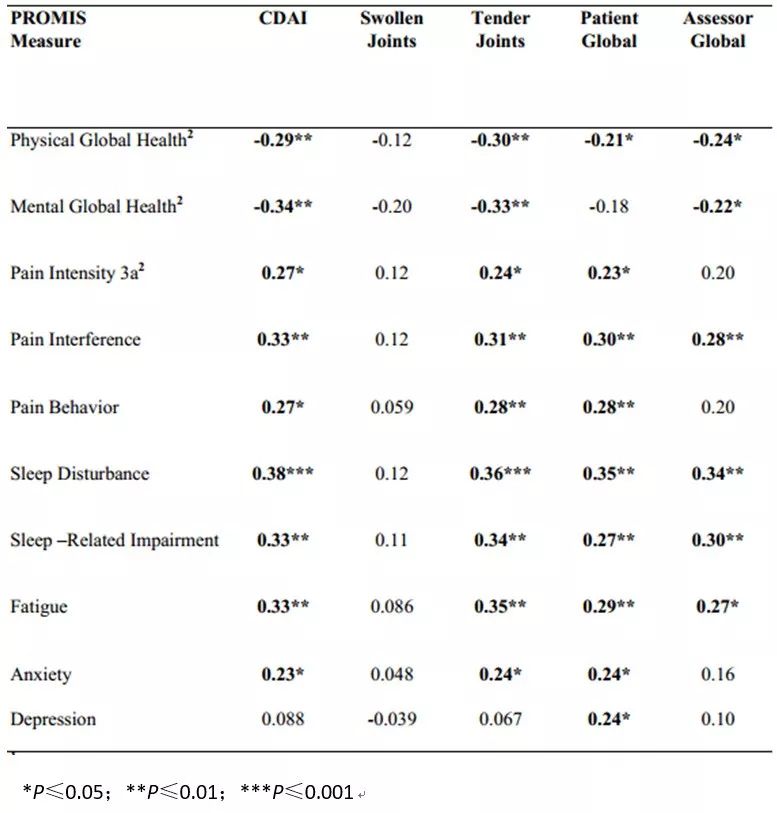
受试者在DMARD治疗启动前后完成了PROMIS 8项指标评估。采用线性回归分析基线PROMIS指标与通过临床疾病活动指数(CDAI)评估的疾病活动度之间的横断面相关性。采用配对t检验评估DMARD治疗12周后的反应性。采用线性回归评估PROMIS指标变化与CDAI变化之间的关联。研究结果显示,156例完成首次研究访视的受试者中,基线CDAI评分均值为25.5 ± 14.0。基线PROMIS整体躯体健康、疼痛和睡眠指标评分与基线CDAI相关(P≤0.05)(表1)。在106例具有12周数据的受试者中,启动DMARD治疗后所有PROMIS评分均改善(P≤0.05)(表2)。除抑郁外,所有评估的PROMES指标改变均与CDAI改变相关(标准化β为|0.23 - 0.38|)(表3)。
表1. 标准化β显示基线PROMIS T-评分与疾病活动度之间的关联(n=156)
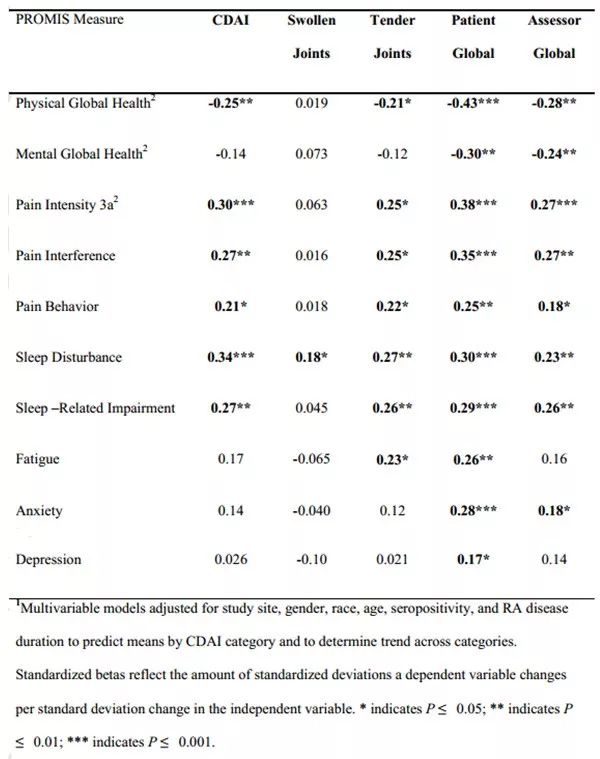
表2. DMARD治疗前后PROMIS T评分(n=106)

表3. 标准化β显示PROMIS T-评分改变与疾病活动度改变之间的关联(n=106)
该研究的优点在于纳入了大样本量的活动性RA患者,并在DMARD治疗后对患者进行了全面评估。该研究的局限性在于缺乏与未启动DMARD治疗的RA患者进行比较;也未评估PROMIS与血清炎性标记物之间的相关性;未纳入躯体功能评估;仅60.9%的受试者在基线访视时使用DMARD。
总之,该研究结果支持PROMIS指标用于评估活动性RA患者的躯体和精神健康。在启动DMARD治疗后,所有PROMIS指标均显著改善,而PROMIS指标变化与CDAI变化存在低中度的关联性。
意义与创新
-
这是首项在启动DMARD治疗的活动性RA患者中采用8个PROMIS计算机适应性测试(CAT)和2个简短量表评估躯体和心理健康的研究。
-
PROMIS指标可以评估接受DMARD治疗的活动性RA患者的整体健康症状、疼痛、睡眠、疲劳和情绪健康变化。
-
DMARD治疗12周后整体躯体健康、整体心理健康、疼痛、睡眠、疲劳和焦虑的PROMIS指标变化与疾病活动度变化显著相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PROM#
46
#Arthritis#
27
#反应性#
32
#ART#
31
#DMARD#
27
#PRO#
24