Blood:PD-1/PD-L1和p53缺失协同促进弥漫性大B细胞淋巴瘤进展
2019-04-13 MedSci MedSci原创
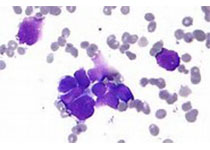
难治性或复发性弥漫性大B细胞淋巴瘤(DLBCL)常与活化的B细胞样(ABC)亚型和驱动NF-kB的固有性激活和影响B细胞的终末分化的基因突变相关。
在ABC-DLBCL中,NF-kB的固有性激活和阻断终末分化可触发p53信号通路和抗肿瘤免疫逃逸机制。
摘要:
难治性或复发性弥漫性大B细胞淋巴瘤(DLBCL)常与活化的B细胞样(ABC)亚型和驱动NF-kB的固有性激活和影响B细胞的终末分化的基因突变相关。
Marién Pascual等人发现,在ABC-DLBCL淋巴瘤发生过程中,p53的DNA损伤反应是抑制IKK2ca介导的经典NF-kB和Blimp1缺失所导致的分化损伤的协同致病作用的中心机制。
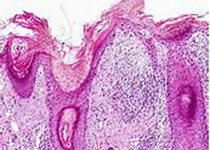
研究人员还发现基因突变和肿瘤微环境(TME)之间的相互作用可选择了促进淋巴瘤进展的其他分子成瘾,包括FOXP1和B细胞诱变酶AID的异常共表达。此外,研究人员还发现肿瘤细胞免疫逃逸是通过下调MHC-II、上调PD-L1和耗竭T细胞来实现的。
PD-1阻滞与抗CD20介导的B细胞毒性具有协同作用,可促进延长T细胞的再激活,提高抗肿瘤的特异性,从而提高小鼠的总体存活率。
总而言之,本研究揭示了DLBCL中NF-kB驱动的促存活、遗传不稳定性和免疫逃逸机制之间的致病性互作,为采用PD-1/PD-L1阻滞联合免疫疗法治疗ABC-DLBCL提供临床支持。
Marién Pascual,et al. PD-1/PD-L1 immune checkpoint and p53 loss facilitate tumor progression in activated B cell diffuse large B-cell lymphomas. Blood 2019 :blood.2018889931; doi: https://doi.org/10.1182/blood.2018889931
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞淋巴瘤#
34
#PD-L1#
28
#B细胞#
42
#弥漫性大B细胞淋巴瘤#
30
#p53#
127
#弥漫性#
30