Nat Biotechnol:新方法有望让造血干细胞移植更加安全
2016-06-09 佚名 生物谷
哈佛大学干细胞研究所(HSCI)的科学家们朝开发出一种让骨髓---造血干细胞---移植更加安全的方法迈出了第一步,也因此能够让数百万患有镰状细胞贫血、地中海贫血和艾滋病等血液疾病的人更加广泛地采用这种疗法。 当前,骨髓移植是这些血液疾病的唯一有效的疗法。但是如果要让新移植的造血干细胞发挥作用,那么存在缺陷的造血干细胞首先被“驱逐”或杀死。要做到这一点就必需要求患者忍受化疗和放疗---在体内的
哈佛大学干细胞研究所(HSCI)的科学家们朝开发出一种让骨髓---造血干细胞---移植更加安全的方法迈出了第一步,也因此能够让数百万患有镰状细胞贫血、地中海贫血和艾滋病等血液疾病的人更加广泛地采用这种疗法。
当前,骨髓移植是这些血液疾病的唯一有效的疗法。但是如果要让新移植的造血干细胞发挥作用,那么存在缺陷的造血干细胞首先被“驱逐”或杀死。要做到这一点就必需要求患者忍受化疗和放疗---在体内的作用比较猛烈,经常产生伴随终生的不良影响。
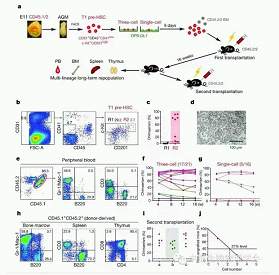
在一项新的研究中,来自哈佛大学、麻省总医院(MGH)、波士顿儿童医院和达纳法伯癌症研究所的研究人员利用抗体特异性地靶向小鼠体内的造血干细胞,开发出一种无毒的移植方法。他们希望这一方法将使得造血干细胞移植对患者的毒性更少。相关研究结果于2016年6月6日在线发表在Nature Biotechnology期刊上,论文标题为“Non-genotoxic conditioning for hematopoietic stem cell transplantation using a hematopoietic-cell-specific internalizing immunotoxin”。
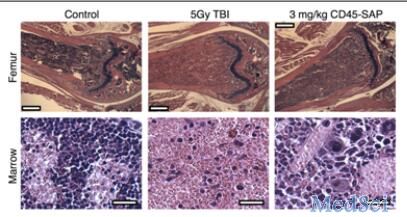
这种新的治疗方法移除小鼠体内98%以上的造血干细胞,这就使得它与化疗和放疗一样有效。
论文通信作者、哈佛大学医学教授和HSCI副主任David Scadden博士说,“我们并没有使用产生大量附带损害的非靶向药物(non-targeted drug),相反,我们能够利用免疫系统特别是抗体的精确靶向作用。”
作为免疫系统的一部分,抗体天然地寻找和破坏体内的外源物质。论文第一作者和Scadden实验室博士后研究员Rahul Palchaudhuri将CD45靶向抗体与只破坏现存的血细胞的装载物(皂草素)装备在一起。这种皂草素通过不同于当前标准疗法的作用方式杀死血细胞。
Palchaudhuri说,“抗体能够特异性地作用于它们的靶标。我们能够让它们靶向作用于CD45,一种只在血液系统中表达的细胞标志物。这样,我们就能够避免对非血液组织产生毒性。”
不同于化疗和放疗---不加区别地对细胞和组织(不论是健康的,还是患病的)造成损伤,CD45靶向抗体不会对胸腺和骨髓---在T细胞和先天性免疫细胞形成中起着至关重要作用的地方---造成伤害。接受这种抗体治疗的小鼠能够抵抗对接受放疗的小鼠而言是致命性的感染。当前,移植后感染是经常发生的,而且可能比较严重,也因此造成相当数量的患者死亡。
在接受标准治疗(化疗或放疗)后,大约十分之一的患者在接受移植后不能存活下来。这些患者可能产生生长发育迟缓、智力发育迟缓、不孕不育和DNA损伤;当前,患者只能够通过增加以后患上癌症的风险尝试进行治疗性移植。
Scadden解释道,正因为如此,家人和医生经常避免选择移植治疗方案,特别是当它涉及小孩治疗时,而且这将限制基因疗法和基因编辑领域取得的突破能够在多大程度上应用。
接受这种抗体治疗的小鼠有10天的窗口期接受骨髓移植,而且没有接受骨髓移植的个别小鼠能够完全康复,没有副作用。再者,利用这种抗体方法进行处理后对患有镰状细胞贫血的小鼠成功地进行移植,能够治愈它们的贫血症。如果这也适用于人类的话,那么住院进行几个月的康复就可能被一种门诊手术取代,而且移植即便失败也不会是致命的。
Scadden说,“如果这种方法也在人体有效的话,那么它将真正地改变医生与病人之间的互动”,特别是那些“患有这些潜在的遗传性疾病的患者,和新的基因编辑和基因治疗技术正在开发中的那些患者。”
如今,研究人员正在试图鉴定出在人体有效的抗体,而且已组建一家公司对这项研究进行临床转化,并且确定哪些动物模型最适合在临床前研究中使用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
30
#新方法#
40
#TEC#
30
#细胞移植#
36
#Nat#
24
#Biotech#
24
的确这样
102
应该学习
113
#造血干细胞#
31
#造血#
29