JAMA Neurol:远程医疗对院前卒中患者的评估和治疗效果
2015-12-29 phylis 译 MedSci原创
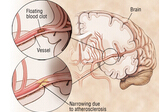
背景:现场治疗处理团队的移动卒中治疗单元(MSTUs)包括可以提供溶栓的血管神经医师。这个单元可以高效利用资源,如果可以依赖远程医疗的话,可以减少对现场神经科医生的需要。
背景:现场治疗处理团队的移动卒中治疗单元(MSTUs)包括可以提供溶栓的血管神经医师。这个单元可以高效利用资源,如果可以依赖远程医疗的话,可以减少对现场神经科医生的需要。
目标:为了测试远程医疗是否是可靠的,以及远程医疗存在对MSTU进行急性卒中治疗是否是足够的。
设计,设置和参与者:2014年7月18日至11月1日间进行的前瞻性观察研究。研究分析的日期是2014年11月1日到2015年3月30日。这是一个以社区为基础的研究,评估俄亥俄州,克利夫兰MSTU中远程医疗的应用。在克利夫兰诊所MSTU项目实施后,受试者是克利夫兰首批100在早上8点和晚上8点之间的脑卒中样症状的急性发作的居民,并进行MSTU评估。血管神经科医师通过远程医疗评估前100患者、神经影像科医生通过CT扫描后对脑影像进行远程评估。医疗记录数据,并将数据记录到一个前瞻性注册表。
主要成果和措施:研究比较了同年,MSTU治疗的患者和通过急诊进行急诊部治疗的患者。记录了患者从发病到进入MSTU治疗或急诊部治疗的患者,并且记录在评估过程中遇到的问题。
结果:成功评估了99/100名患者。远程医疗评估时间的中位数为20分钟(IQR,14-27分钟)。一个患者由于联系的失误被运送到最近的急诊科。6名患者远程医疗联接失败,但持续未超过60秒,临床护理并未受到影响。MSTU组从开始到CT完成时间(13分钟,IQR :9-21分钟),从开始到静脉溶栓(32分钟, IQR 24-47分钟)的时间短于对照组(18分钟,IQR:12-26分钟)和( 58分钟,IQR:53-68分钟)。对CT的判断的时间,两组间没有差异。
结论与相关性:MSTU中应用远程医疗是可行的,技术失败率较低,并且为降低系统成本提供了途径。
原文出处:
Itrat A, Taqui A, et al. Telemedicine in Prehospital Stroke Evaluation and Thrombolysis: Taking Stroke Treatment to the Doorstep. JAMA Neurol. 2015 Dec 7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#卒中患者#
20
#院前#
27
#Neurol#
19
#治疗效果#
28
学习!
98
了解
99