各科诊断公式大全(医学知识,可收藏)
2015-02-17 MedSci 医学之声
呼吸系统疾病诊断公式 1.急性上呼吸道感染=咽痛+咳嗽+发热 2.肺炎 (1)大叶性肺炎=成人+受凉+高热+咳铁锈色痰 (2)克雷伯杆菌肺炎=咳砖红色痰+X线片空洞 (3)支原体肺炎=儿童+刺激性干咳+关节疼+抗生素无效 (4)支气管肺炎=婴幼儿+发热+呼吸困难症状(鼻翼扇动、三凹征阳性) (5)金色葡萄球菌肺炎=高热+胸痛+脓血痰+X线片状影 3.结核病 (1)肺结核=青壮年+
呼吸系统疾病诊断公式
1.急性上呼吸道感染=咽痛+咳嗽+发热
2.肺炎
(1)大叶性肺炎=成人+受凉+高热+咳铁锈色痰
(2)克雷伯杆菌肺炎=咳砖红色痰+X线片空洞
(3)支原体肺炎=儿童+刺激性干咳+关节疼+抗生素无效
(4)支气管肺炎=婴幼儿+发热+呼吸困难症状(鼻翼扇动、三凹征阳性)
(5)金色葡萄球菌肺炎=高热+胸痛+脓血痰+X线片状影
3.结核病
(1)肺结核=青壮年+咯血+午后低热+夜间盗汗+抗生素治疗无明显疗效
(2)结核性胸膜炎=结核+胸膜积液体征(胸痛+语颤消失+叩诊实音/呼吸音消失)
(3)结核性心包炎=结核+心包积液体征(心前区痛+呼吸困难+上腹部闷胀+下肢浮肿)
(4)肠结核=结核+腹部症状(腹痛、腹泻、右下腹部肿块)
(5)结核性腹膜炎=结核+腹部炎症(腹痛、腹泻、腹壁柔韧感)
(6)肾结核=结核+膀胱刺激征+肾实质变薄并有破坏
4.支气管扩张=童年有麻疹百日咳或支气管肺炎迁延不愈病史+咳嗽+脓痰+咯血
5.COPD=老年人(吸烟史)+咳痰喘+桶状胸+肺功能检查,一秒率FEV1/FVC%小于
6.肺脓肿=脓臭痰+高热+X线片/CT显示液平
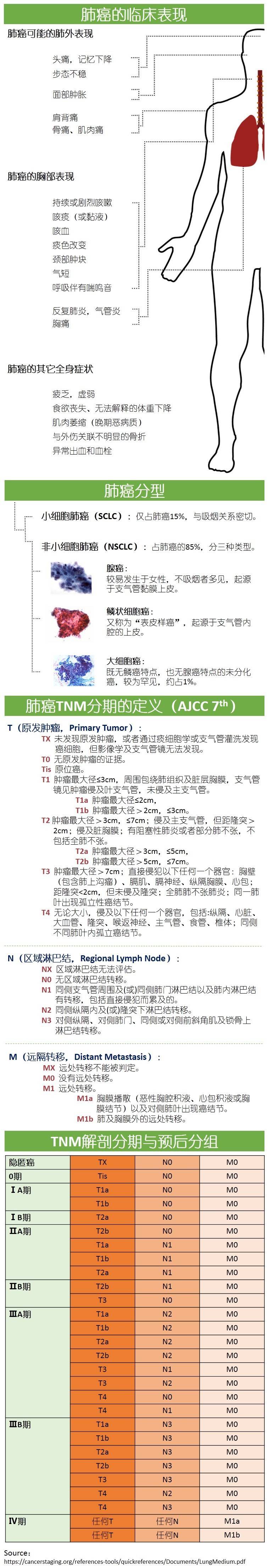
7.肺癌=中、老年人+痰中带血+刺激性咳嗽+消瘦+X线毛刺
8.肺心病=慢性肺部疾病病史+心脏扩大
演变顺序:慢支-肺气肿-肺心病
9.支气管哮喘=阵发性或周期性喘息+听诊哮鸣音+过敏史
10.呼吸衰竭=慢性肺部疾病病史+发绀+血气分析指标
I型:PaO2<60mmHgPaCO2正常-重症肺炎诱发
II型:PaO2<60mmHgPaCO2>50mmHg-慢阻肺诱发
11.胸部闭合性损伤
(1)张力性气胸=胸外伤史+广泛皮下气肿(握雪感)+气管偏移+叩诊鼓音+呼吸音消失
(2)血胸=胸外伤史+气管偏移+叩诊浊音+呼吸音减弱+X线肋膈角消失,弧形高密度影
(3)肋骨骨折=胸外伤史+骨擦音
1.胸部X片、胸部
2.PPD、血沉
3.痰培养+药敏实验、痰找结核杆菌
4.肺功能
5.肝肾功能
6.血气分析
7.纤维支气管镜
8.痰液脱落细胞检测
9.淋巴结活检
10.血常规、电解质
呼吸系统疾病治疗原则
1.一般治疗:休息,加强营养,预防感染/吸氧
2.对症治疗/药物治疗
(1)抗感染治疗:使用广谱抗生素或联合用药
(2)抗结核治疗:早期、适量、联合、规律、全程
(3)抗休克:扩容,使用血管活性药物
(4)控制咯血:垂体后叶素
(5)解热、止咳、平喘、祛痰
(6)纠正酸碱平衡失调
3.肿瘤(肺癌)
(1)手术治疗
(2)放疗+化疗+免疫治疗+中医中药治疗
消化系统疾病诊断公式
1、急慢性胃炎=饮食不洁或刺激物+上腹痛、腹胀、恶心、呕吐
2、胃食管反流病=反酸+胸骨后烧灼感+胃镜检查食管下端红色条状糜烂带(烧心、反酸、返食)
3、消化性溃疡病:
胃溃疡=慢性规律性上腹痛(饱餐后痛)+呕血黑便
十二指溃疡=饥饿时痛(餐后4小时以上)或夜间痛+呕血黑便
4、食管胃底静脉曲张=上消化道大出血+既往肝病史
5、细菌性痢疾=不洁饮食+腹痛+粘液脓血便+里急后重
6、溃疡性结肠炎=坐下腹痛+粘液脓血便+(便意、便后缓解)+抗生素治疗无效治疗:柳氮磺吡啶
7、急性胰腺炎(水肿型)=暴饮暴食、慢性胆道病史+持续上腹痛+弯腰疼痛减轻+淀粉酶检测
急性胰腺炎(出血坏死性)=水肿性症状+腰肋部或脐周紫斑+腹穿息肉水样液体+血糖高+血钙低(血尿淀粉酶值不一定高,有时反而下降。确诊需要选CT。)
胰腺炎一周内查血淀粉酶,超过一周测脂肪酶。
8、幽门梗阻=呕吐宿食+振水音
9、肝硬化=肝炎病史+门内脉高压(脾大+腹水+蜘蛛痣)+超声(肝缩小)
10、胆囊炎=阵发性右上腹绞痛+墨菲氏征阳性+恶心呕吐
11、胆石症=阵发性右上腹绞痛+墨菲氏征阳性+B超强回声光团、声影
12、急梗化(急性梗阻性化脓性胆管炎)=夏柯三联征(腹痛+寒战高热+黄疸)+休克表现+精神症状(如;表情淡漠、昏迷)五联症
13、急腹症
(1)阑尾炎=转移性右下腹痛+麦氏点压痛(胀痛、闷痛)+WBC高
(2)肠梗阻;腹痛、吐、胀、闭+X线(香蕉/液平)
病因:机器性和动力性
血运:单纯性和绞窄性
程度:完全性和不完全性
部位:高位和低位
(3)消化道穿孔=溃疡病史+突发上腹部剧痛+腹膜刺激征+膈下游离气体
(4)异位妊娠=阴道出血+停经史+下腹剧痛(宫颈举痛)+绒毛膜促性腺激素(+)
(5)卵巢囊肿提扭转=体位变化+突发腹痛+囊性肿物
(6)急性盆腔炎=刮宫手术史+白带异常+下腹痛+下腹剧痛(宫颈举痛)+脓性分泌物
14、消化道肿瘤
(1)胃癌=老年人+黑便+龛影+慢性溃疡疼痛规律改变+上腹痛+腹部包块+消瘦+左锁骨上淋巴结肿大
(2)食管癌=进行性吞咽困难(中晚期)+胸骨后烧灼样疼痛(早期)+进食哽噎感(早期)
(3)肝癌=肝炎病史+肝区疼痛+AFP高+肝大质硬+腹水黄疸+B超占位
(4)直肠癌=直肠刺激症状+指诊带血+脓血便+消瘦+大便变化
(5)胰腺癌(胰头癌、壶腹周围癌)=老年人+无痛性进行性加重黄疸+陶土色大便+皮肤瘙痒
(6)结肠癌=老年人+消瘦+排便习惯管改变+CEA+腹部肿块(左、溃疡性/右,肿块型)
15、肛门、直肠良性病变
(1)内痔=无痛性血便+便带鲜血+静脉样团块
(2)外痔=肛门疼痛+便鲜血+肛门口触痛肿物
(3)肛裂=便时便后肛门剧痛+肛门裂口
16、腹部闭合性损伤
肾损伤=腰部损伤+血尿
肝破裂=右腹部外伤+腹膜刺激征+移动性浊音
脾破裂=左腹部外伤+全腹痛+腹腔内出血
肠破裂=腹中部外伤+腹膜刺激征+穿刺淡黄色液体
17、腹外疝
斜疝=老年男性+腹压增高+右下腹肿物+进入阴囊
1、胃镜、结肠镜、直肠镜
2、消化道造影
3、腹部B超、
4、立位腹平片
5、粪便:常规检查、隐血、培养和寄生虫检查
6、HP检查
7、腹腔穿刺
8、淋巴结活检或肝活检(病理监测)
9、实验室检查:
(1)血尿淀粉酶
(2)AFP、CEA、CA19-9糖链抗原
(3)血尿常规、肝功肾功、电解质、血气分析等
一、一般治疗:注意休息,控制饮食、禁食,生活指导
二、病因治疗
(1)溃疡:首选PPI类抑酸药,可加用黏膜保护剂,如有幽门螺旋菌感染应联合除菌治疗,常用三联或四联疗法;PPI/胶体铋联合两种抗生素。
(2)应用广谱抗生素抗感染治疗、抗休克治疗
(3)梗阻/腹膜炎:禁食、胃肠减压
(4)为维持水电解质酸碱平衡
三、对症治疗
四、手术:切除或修补
五、肿瘤
1)手术治疗
2)放疗+化疗+免疫治疗+中医中药治疗
1.冠心病=胸骨后压窄性疼痛
(1)心绞痛=胸骨后压窄性疼痛<30分钟,3-5分钟/次,+休息或口含硝酸甘油能缓解+ECG:ST段水平下移
(2)心梗=胸骨后压窄性疼痛>30分钟,休息或口含硝酸甘油不能缓解+大汗淋漓+濒死感+ECG:ST段弓背向上抬高
V1-6广泛前壁心梗
V1-3前间壁心梗
V3-5局限前壁心梗
V5-6前侧壁心梗
Ⅱ、Ⅲ、aVF下壁心梗
I、aVL高侧壁心梗
心功能Killip分级:用于评估急性心肌梗死患者的心功能状态
I级:无肺部啰音和第三心音
II级:肺部有啰音,但啰音的范围小于1/2肺野
III级:肺部啰音的范围大于1/2肺野(肺水肿
IV级:心源性休克
2.高血压病
按患者的心血管危险绝对水平分层(正常140/90)
1级140-159或90-99低于
2级160-179或100-109低于
3级≥180或≥
危险程度分层
低危:1级。改善生活方式。
中危:1级+2个因素;2级不伴或低于2个因素。药物治疗。
高危:1-2级+至少3个因素,靶器官损害。规则药物治疗。
极高危:3级;1-2级+靶器官损害、有并发症。尽快强化治疗。
3.心衰=左肺(循环)右体(循环)
左心衰=咳粉红色泡沫样痰+呼吸困难(夜间不能平卧、端坐呼吸、活动后)
右心衰=颈静脉怒张+双下肢水肿+肝大
心功能分级
I级日常不受限
II级活动轻度受限
III级活动明显受限
IV级休息时出现症状
左心衰+右心衰=全心衰
4.心律失常:
(1)房颤=心律绝对不等+脉短绌+心电图f波+第一心音强弱不等
(2)阵发性室上性心动过速=阵发性心慌+突发突止+ECG(无P波,心率160-250次/分)
(3)阵发性室性心动过速=突发性心慌+既往发作史+ECG连续3次以上的快速宽大畸形的QRS波+心室夺获/室性融合波
(4)其他:见第三站心电图学部分
5.心脏瓣膜病
(1)二尖瓣狭窄=呼吸困难(劳力性、阵发性、夜间、端坐呼吸、急性肺水肿)+急性大量咯血、粉红色泡沫痰+梨形心+隆隆样杂音
(2)二尖瓣关闭不全=急性左心衰/慢性晚期出现左衰或全衰+心尖部粗糙的全收缩期吹风样杂音,向腋下或左肩胛下角传导
(3)主动脉瓣狭窄=呼吸困难+心绞痛+晕厥+喷射性杂音并向颈部传导
(4)主动脉瓣关闭不全=心悸+心绞痛+夜间阵发性呼吸困难+AustinFliht杂音+周围血管征(水冲脉、Mussctz征、颈动脉波动明显、毛细血管搏动征、动脉枪击音及Durozicz征)
主要瓣膜杂音出现时期开关瓣杂音性质
二尖瓣狭窄舒张期开隆隆样
二尖瓣关闭不全收缩期关吹风样
主动脉瓣狭窄收缩期开喷射样
主动脉瓣关闭不全舒张期关叹气样
6.休克体征=P↑+Bp↓+脉搏细速+四肢发凉
(1)失血性休休克体征+出血
(2)心源性休克=休克体征+左心衰
1.心电图、动态心电图
2.超声心动图
3.胸部X线
4.眼底检查(高血压)、放射性核素
5.心肌酶谱
6.血气分析
7.血常规、血脂、血糖、血钾、肝肾功能
8.心导管
9.冠脉造影
10.心肌坏死标记物(肌红蛋白、肌钙蛋白、肌酸激酶同工酶CK-MB)
1.一般治疗:注意休息、改变生活方式(如戒烟酒、低钠低脂饮食、适度运动),检测,护理
2.高血压:
(1)利尿剂、B受体阻滞剂、钙通道阻滞剂、ACEI(血管紧张素转换酶抑制剂)、血管紧张素II受体阻滞剂
(2)控制合并症。如心衰、糖尿病、脑血管病、肾衰、冠心病
3.冠心病:
对症治疗:控制心律失常,改善心功能,心梗II预防
溶栓或介入治疗
控制休克,纠正心衰
抗凝及抗血小板药物治疗:阿司匹林、肝素
4.房颤:
药物复律,选用胺碘酮
减慢心室率,选用西地兰
5.心衰:
利尿、ACEI、B受体阻滞剂、正性肌力药(洋地黄类:地辛高、西地兰。非洋地黄类:多巴胺、米力农)、心脏起搏器
6.瓣膜病:
病因治疗、瓣膜置换等
1.肾小球肾炎:眼睑/颜面部水肿+青少年+链球菌感染史+C3下降+血尿蛋白尿高血压
2.尿路感染
(1)肾盂肾炎=女性+腰痛+发热+脓尿、白细胞管型
(2)慢性肾盂肾炎急性发作=尿路损伤史+膀胱刺激征反复发作+腰痛+发热+肾区叩击痛+WBC升高
(3)下尿路感染=已婚女性+发热+膀胱刺激征
3.肾结石=活动后出现血尿+腰部绞痛+B超或X线
4.输尿管结石=活动后出现血尿+腰部绞痛+X线检查
5.肾癌=老年人+(无痛性)肉眼血尿
6.肾衰=多年肾炎病史+血尿蛋白尿高血压+血肌酐(代偿期133、失代偿期442、衰竭期707、尿毒症期)升高
7.前列腺增生=老年人+尿频+进行性排尿困难
1.腹部B超、平片
2.血尿常规、血沉、肾功能、血气分析
3.肾盂造影
4.穿刺活检
5.妇科检查
6.血肌酐、肾小球滤过率
7.肾功能
8.放射性核素肾图
9.膀胱镜
1.一般治疗:注意休息、低钠/低蛋白饮食
2.对症治疗
(1)抗感染
(2)利尿降压
(3)透析
(4)纠正水电解质酸碱失调
3.外科治疗:手术切除或切开
4.肿瘤(肾癌)
5.血液透析治疗
1.白血病=发热+出血倾向+胸骨压痛+全血细胞减少
2.再生障碍性贫血=贫血貌+出血倾向+三系减少
3.自身免疫性溶血性贫血=贫血貌+Coombs(抗人球蛋白实验)阳性+脾大
4.缺铁性贫血=血清铁下降+贫血貌(皮肤黏膜苍白)+女性月经过多或消化系统肿瘤
5.特发性血小板减少紫癜=女性+出血倾向+血小板降低(小于100-109),红白细胞计数正常
6.DIC=多部位出血+PT延长+3P试验阳性
血液系统疾病进一步检查:
1.骨髓穿刺检查
2.细胞形态学检查
3.肝肾功能、腹部B超
4.血常规
一般治疗:休息,控制感染,选用广谱抗生素
白血病:化疗+骨髓移植
化疗:
急性白血病,急淋-DVLP方案
(柔红霉素、长春新碱、左旋门冬酰胺酶、泼尼松)
急非淋-DA方案
(柔红霉素、阿糖胞苷)
早幼粒-维甲酸
慢性白血病
自身免疫性溶血性贫血:糖皮质激素,脾切除
TTP:糖皮质激素,脾切除
再障:雄激素,免疫制剂,骨髓移植
贫血:补充铁剂+VC,手术前贫血严重可输注红细胞
1.脑出血=老年患者+高血压病史+急性起病+意识障碍+定位体征
2.脑血栓=安静状态发病(冠心病、高脂血症)
3.脑栓塞=发病急+心脏栓子(亚急性心内膜炎)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好资料
66
不错学习并分享了谢谢
53
很不错学习了
114
背下来
158
?
129
受用
108
收藏啦
78
没细看,先收藏了
44
收藏
85
不错的文章,学习了
86