Diabetic Med:成人护理提供者对1型糖尿病年轻患者向成人护理过渡的观点如何?
2018-10-24 MedSci MedSci原创
近日,国际杂志 《Diabetic Med》上在线发表一项关于成人护理提供者对1型糖尿病年轻患者向成人护理过渡的观点的一项跨部门调查的研究。研究目的是评估成人糖尿病护理提供者者目前的过渡实践,过渡护理知识,以及对1型糖尿病年轻患者的过渡护理中实施最佳实践的障碍。 研究人员通过魁北克内分泌医学协会和魁北克糖尿病协会对成人糖尿病护理提供者进行了38项基于网络的调查。53名医生做出了回应(35%)
近日,国际杂志 《Diabetic Med》上在线发表一项关于成人护理提供者对1型糖尿病年轻患者向成人护理过渡的观点的一项跨部门调查的研究。研究目的是评估成人糖尿病护理提供者者目前的过渡实践,过渡护理知识,以及对1型糖尿病年轻患者的过渡护理中实施最佳实践的障碍。
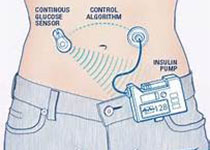
研究人员通过魁北克内分泌医学协会和魁北克糖尿病协会对成人糖尿病护理提供者进行了38项基于网络的调查。53名医生做出了回应(35%)。不到一半的受访者(46%)熟悉美国糖尿病协会的过渡期护理共识。大约三分之一的受访者表示儿科和成人糖尿病护理之间存在> 6个月的差距。大多数人(83%)认为与儿科团队的沟通是充分的; 然而,只有56%的人报告接受了医疗总结,2%的儿童医疗服务者提供心理社会总结。受访者认为,儿科团队应该通过发展自我管理技能,改善儿科和成人护理之间的差异,从而改善对过渡护理的准备。只有31%的具有一个系统来识别在成人护理中丢失的对年轻患者的随访。感知障碍包括难以获得心理社会服务,新出现的动力缺乏以及过渡准备不足。大多数(87%)有兴趣拥有额外的资源,包括自我管理工具和注册表来对那些失去后续行动的人进行随访。
研究结果强调需要更好地让成人护理提供者参与过渡护理实践。尽管成人医生对转型护理感兴趣,但过渡护理建议和临床护理资源的实施仍然有限。因此需要加强努力以改善成人医疗环境中获得精神卫生服务的机会。
原始出处:
S. Michaud, K. Dasgupta, L. Bell,et al. Adult care
providers’ perspectives on the transition to adult care for emerging adults
with Type 1 diabetes: a cross‐sectional survey
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIA#
24
#Diabetic#
35
#BET#
29
#年轻患者#
34
#Med#
33
谢谢MedSci提供最新的资讯
33