Int J Cardiol:CHA2DS2-VASc评分与ACS患者冠状动脉疾病的严重程度、残余血小板反应性和长期临床结局的关系!
2018-03-21 xing.T MedSci原创
在ACS患者的队列中,CHA2DS2-VASc评分与冠状动脉疾病的严重程度和残余血小板反应性相关,因此,它可预测不良事件的长期风险。
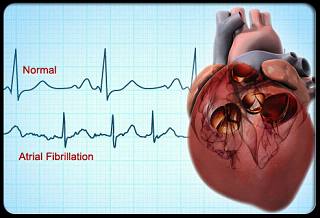
CHA2DS2-VASc评分可预测房颤患者卒中风险,但最近有报道其在ACS患者中具有预后作用。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员试图评估CHA2DS2-VASc评分预测冠状动脉病变严重程度、高残留血小板反应性和急性冠状动脉综合征(ACS)患者长期结局的能力。
总的来说,该研究纳入了1729名连续就诊的接受侵入性治疗的ACS患者。研究人员通过氯吡格雷负荷后的透光率集合度测定评估了血小板反应性。根据CHA2DS2-VASc评分患者被分为:A组 = 0、B = 1、C = 2、D = 3、E = 4和F ≥ 5。
CHA2DS2-VASc评分较高的患者更有可能发生冠状动脉多支病变(对于A、B、C、D、E和F组分别为37%、47%、55%、62%、67和75%;P < 0.001);此外,CHA2DS2-VASc评分与残余血小板反应性呈线性相关(r = 0.77;P<0.001)。在长期随访过程中,A、B、C、D、E和F组估计的不良事件(MACCE:心源性死亡、米河、卒中或任何紧急冠状动脉血运重建)发生率分别为3%、8%、10%、14%、19%和24%,P<0.001。多变量分析显示CHA2DS2-VASc评分是冠状动脉病变严重程度、高残留血小板反应性和MACCE的独立预测因子。
在ACS患者的队列中,CHA2DS2-VASc评分与冠状动脉疾病的严重程度和残余血小板反应性相关,因此,它可预测不良事件的长期风险。
原始出处:
Fernando Scudiero,et al. Relationship between CHA2DS2-VASc score, coronary artery disease severity, residual platelet reactivity and long-term clinical outcomes in patients with acute coronary syndrome.International Journal of Cardiology.2018. https://doi.org/10.1016/j.ijcard.2018.03.086
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#反应性#
22
#ASC#
20
#临床结局#
0
#Cardiol#
30
#CHA2DS2-VASc评分#
37
#血小板反应性#
26
#CHA2#
33
#冠状动脉疾病#
24
#ACS#
30
#CHA2DS2-VASc#
22