JACC:房颤复律患者抗凝:阿哌沙班PK华法林(ARISTOTLE研究)
2014-04-13 MedSci MedSci原创
房颤患者心脏复律后可能发生栓塞事件。对于房颤持续<48小时的患者,当前指南推荐至少在心 脏复律前3周和复律后4周给予抗凝治疗,是INR维持在2.0-3.0。维生素K拮抗剂和达比加群或可降低复律后栓塞风险。那么,同为新型抗凝药的Xa因 子抑制剂阿哌沙班是否能够降低这种风险呢?阿哌沙班和华法林相比,哪个更好呢?为此,研究者对ARISTOTLE试验中复律患者的数据进行了事后分析,旨在确定房颤复律后服
房颤患者心脏复律后可能发生栓塞事件。对于房颤持续<48小时的患者,当前指南推荐至少在心 脏复律前3周和复律后4周给予抗凝治疗,是INR维持在2.0-3.0。维生素K拮抗剂和达比加群或可降低复律后栓塞风险。那么,同为新型抗凝药的Xa因 子抑制剂阿哌沙班是否能够降低这种风险呢?阿哌沙班和华法林相比,哪个更好呢?
为此,研究者对ARISTOTLE试验中复律患者的数据进行了事后分析,旨在确定房颤复律后服用阿哌沙班与华法林主要临床和血栓栓塞事件风险。
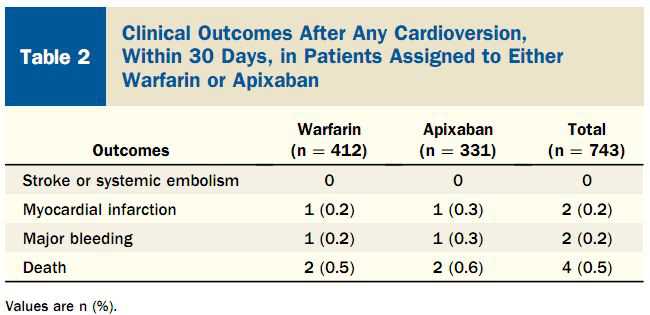
ARISTOTLE试验中,540例患者共有743次心脏复律:将首次复律的患者随机分配到阿哌沙班组(n=265)和华法林组(n=275);两组从首次复律到随机分配的时间分别为243±231天和251±248天;75%的心脏复律发生在1年。两组基线特征相似。
在随访30天中,接受复律的患者未发生卒中和系统性栓塞。华法林组和阿哌沙班组各有1例发生心肌梗死(0.2%,0.3%),各有1例主要出血事件(0.2%,0.3%)和2例死亡(0.5%,0.6%)。
房颤复律后主要心血管事件非常罕见,两组发生率相似。
附图:
参考文献:
Flaker G, Lopes RD, Al-Khatib SM, Hermosillo AG, Hohnloser SH, Tinga B, Zhu J, Mohan P, Garcia D, Bartunek J, Vinereanu D, Husted S, Harjola VP, Rosenqvist M, Alexander JH, Granger CB; ARISTOTLE Committees and Investigators.Efficacy and Safety of Apixaban in Patients After Cardioversion for Atrial Fibrillation: Insights From the ARISTOTLE Trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation).J Am Coll Cardiol. 2014 Mar 25;63(11):1082-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









期待有更多的研究
54
#JACC#
32
#ARISTOTLE#
33
#ACC#
36