OCC2018:梁春:独立于降低LDL-C的抗炎治疗,开启抗动脉粥样硬化精准治疗新纪元——CANTOS研究解读
2018-06-04 国际循环编辑部 国际循环
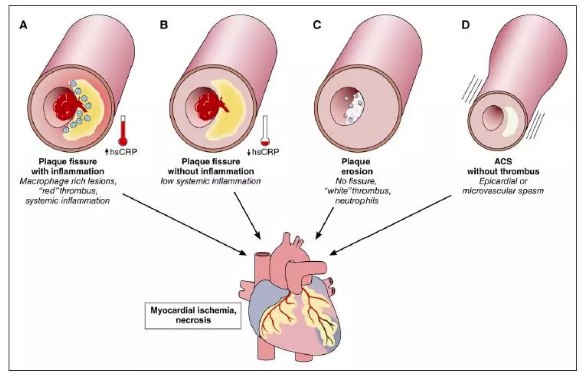
动脉粥样硬化炎症假说,似乎为动脉粥样硬化病变的胆固醇理论提供了重要补充。OCC 2018大会,上海长征医院心血管内科梁春教授从动脉粥样硬化(Atherosclerosis,AS)精准治疗的独特视角,介绍了AS抗炎治疗新机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
19
#新纪元#
33
#抗炎治疗#
31
#精准治疗#
54
#OCC#
22
#精准#
17
#LDL#
20
了解一下.谢谢分享!
51