Lancet:“毛骨悚然”的颅骨——案例报道
2016-10-16 MedSci MedSci原创
患者女,29岁,2014年4月因头痛行了头颅MRI,结果显示板障空间扩大、颅骨外板位移、灰质低信号(T1加权像)。 患者的头颅X片出现“竖毛征”,骨小梁栅栏状改变沿颅底骨垂直排列。 既往有先天性纯红细胞再生障碍性贫血III型史。需要定期输血,直到9岁行了脾切除。此后患者每年随访血红蛋白,稳定在90–100 g/L。 先天性纯红细胞再生障碍性贫血是一种罕见的遗传性疾病,以无
患者女,29岁,2014年4月因头痛行了头颅MRI,结果显示板障空间扩大、颅骨外板位移、灰质低信号(T1加权像)。
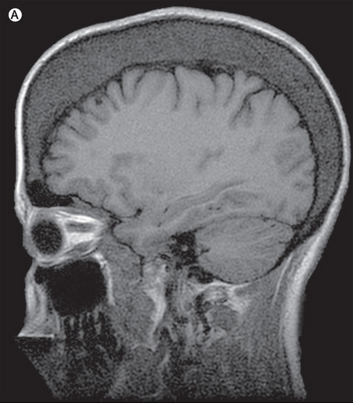
患者的头颅X片出现“竖毛征”,骨小梁栅栏状改变沿颅底骨垂直排列。
既往有先天性纯红细胞再生障碍性贫血III型史。需要定期输血,直到9岁行了脾切除。此后患者每年随访血红蛋白,稳定在90–100 g/L。
先天性纯红细胞再生障碍性贫血是一种罕见的遗传性疾病,以无效红细胞生成为特征。
“竖毛征”见于重度贫血患者。本案例患者的头骨变化是由于因为慢性贫血所致骨髓红细胞生成增加和骨髓增生。
除了上述,患者的MRI没有发现其他异常,诊断为紧张性头痛,使用镇痛药和行为治疗后,完全缓解。
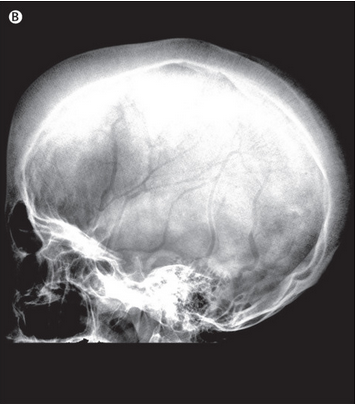
为了加深印象,再给大家看一张其他患者的“竖毛征”CT图像。
原始出处:
María Asunción Pérez-Jacoiste Asín,et al.Skull erythropoiesis in a patient with congenital dyserythropoietic anaemia.Lancet.20 February 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Lancet#
35
第一次见,学习了
67
真是让我毛骨悚然!
56
分析透彻,讲解到位,学习新知识了……
68
很好,不错,以后会多学习
0
很受益,谢谢
64
谢谢指点学习了
39
天下之大,第一次听说
25