导航引导下神经内镜导引器辅助脑室内肿瘤切除
2019-08-10 刘磊 赵艺宁 杨佳 中国神经精神疾病杂志
脑室内肿瘤位置深,暴露困难,常常需对正常脑组织进行牵拉,易导致脑挫伤、血肿形成、癫痫、神经功能缺陷、认知障碍等并发症。既往曾有少量研究报道使用内镜导引器辅助,对此类肿瘤进行切除,与传统手术相比,这种手术方式损伤更小。我们采用自主研发的神经内镜导引器系统,并辅以小骨瓣开颅术在导航下应用内镜对脑室内肿瘤进行切除,现报告如下。
脑室内肿瘤位置深,暴露困难,常常需对正常脑组织进行牵拉,易导致脑挫伤、血肿形成、癫痫、神经功能缺陷、认知障碍等并发症。既往曾有少量研究报道使用内镜导引器辅助,对此类肿瘤进行切除,与传统手术相比,这种手术方式损伤更小。我们采用自主研发的神经内镜导引器系统,并辅以小骨瓣开颅术在导航下应用内镜对脑室内肿瘤进行切除,现报告如下。
1.资料与方法
1.1研究对象
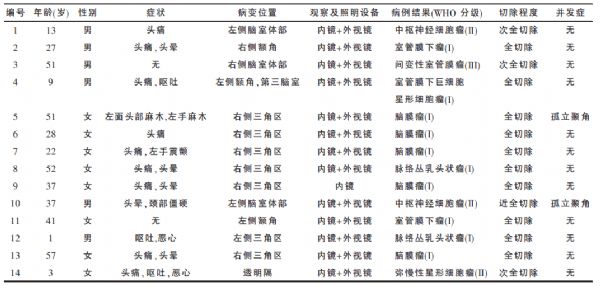
回顾性收集2013年1月至2015年2月解放军总医院神经外科接受内镜辅助下脑室内肿瘤(肿瘤主体位于侧脑室、三脑室,与周围正常脑组织边界清楚、良性可能性大)切除的14例患者资料。其中男6例,女8例,年龄1~57岁。14例患者中有12例表现为头痛、恶心、呕吐等颅高压症状,2例患者为查体发现颅内肿瘤。见表1。1例患者仅使用内镜,其余13例均使用内视镜和外视镜进行手术。本研究已征得患者同意及伦理委员会审核。
表1 14例导航下导引器手术患者的基本信息
1.2方法
收集患者术前症状,病变大小、位置,切除程度及病理结果,术后随访评估患者神经功能状态及术后生活质量。
1.3手术方法
患者术前一天常规进行增强核磁共振扫描,并制定多模态导航计划。本组病例均使用内镜导引器(国家发明专利ZL201210066281.1,欣创通,北京缙铖医疗科技有限公司)。患者全麻后进行神经导航注册,根据导航设计切口及穿刺道,避开重要的神经纤维束及血管。采用4 cm长直线形切口和直径为2 cm的小骨瓣开颅。
将导航注册参考架固定在导引器导芯的末端并对导芯进行注册用于导航(图1A)。在神经导航引导下,用穿刺导芯(直径10mm)进行脑室穿刺(图1B)。穿刺脑室成功后,将导引器透明工作外鞘(直径16mm)沿导芯并对穿刺道再次扩张,并放置到目标位置(图1C)。然后去除穿刺导芯,并用自动牵开器蛇形拉钩夹持导引器固定翼,对工作导引器进行固定。通过工作导引器的外鞘,使用内镜/外视镜及标准的双手显微操作对肿瘤进行切除。对于直径大于工作导引器直径(1.6 cm)的肿瘤,采取分块切除的方式将病变切除。在完成最大安全切除后缓慢移除工作导引器,穿刺通道填塞明胶海绵。硬膜水密缝合后,小骨瓣复位固定,常规关颅。

图1 术中导航辅助下使用导引器操作示意图。A:在导引器导芯(黄色)上端安装导航架,并将导芯注册至导航系统中,使其成为导航工具;B:在导航指引下,应用导芯(直径10mm)按预设穿刺道穿刺脑室内病变;C:将事先安放于导芯上端的透明工作导引器(直径16mm,如B中安放)沿导芯放入脑室,缓慢扩张穿刺道,抵达脑室内病变表面;D:移除导芯和工作导引器上翼,轻柔调整好工作导引器后,用自动牵开器连接下翼,固定工作导引器。
1.4评估方法
肿瘤切除程度使用iPlan3.0(BrainLab,Feldkirchen,德国),根据患者术前、术后的MRI分别进行肿瘤三维重建及量化评估。对病变进行重建时,选取相对适合的序列来进行肿瘤描绘。随访时间1~24个月(中位随访时间6个月),分别进行临床症状及影像学随访,记录统计手术技术相关并发症。
1.5手术结果
患者均完成术后随访,11例患者经术后MRI检查确认全切除或近全切除,3例患者为次全切除。患者术后均无脑积水、偏瘫、感染、癫痫等并发症。有2例肿瘤全切除患者分别在术后6个月和8个月发生了手术侧孤立颞角,影像学检查提示为术侧侧脑室三角区粘连导致孤立颞角。该2例患者接受二期内镜下孤立颞角造瘘及支架植入术,使颞角与同侧侧脑室体部沟通,均获得治愈。

图2 位于左侧额角及三脑室的室管膜下巨细胞星形细胞瘤。A、B、C:为患者术前轴位、冠状位、矢状位增强磁共振影像扫描影像,可见一巨大病变位于左侧额角及第三脑室内,形状不规则;D:标准自动牵开器与工作导引器下翼连接,固定透明的工作导引器;E:成功穿刺左侧额角后,透过透明的工作导引器可见粉红色分叶状病变;F:应用双手的显微操作技术,使用双极电凝和泪滴形吸引器,在外视镜观察及照明下将脑室内肿瘤切除;G、H、I:患者术后1个月复查的轴位、冠状位、矢状位头颅增强磁共振影像扫描影像,提示肿瘤全切除,脑组织回退良好,穿刺道狭窄(白色箭头示)。
1.6典型病例
男性患者,9岁,因剧烈头痛、呕吐2周入院。CT和MRI提示左侧脑室及三脑室内巨大占位,病变均匀强化,且阻塞左侧室间孔导致脑积水(图2A-C)。在神经导航辅助下,使用内镜和外视镜(图2D-F)进行了内镜导引器辅助手术。术后患者高颅压症状迅速好转,术后影像资料确认肿瘤全切除(图2G-I),病理结果为室管膜下巨细胞型星形细胞瘤。术后12个月随访,患者恢复良好,无新发神经功能障碍,无肿瘤复发。
2.讨论
近年来,有报道使用内镜导引器对脑室内肿瘤进行切除,其病变切除率与并发症发生率与本研究中结果较为一致。这表明,使用这种新型导引器并配合使用内镜/外视镜,可有效的用于脑室内肿瘤切除。目前市售常见内镜导引器均是一步穿刺脑组织,并将通道扩张至工作直径(通常为1.5~2.0 cm),较为粗暴,不能达到逐步扩张手术通道的效果,易导致邻近脑组织挫伤。
在本研究中使用的新型导引器系统,分两部穿刺脑组织并对穿刺道进行逐步扩张,能够减小一次性扩张手术通道对周围脑组织的损伤,从而降低对周围脑组织造成挫伤的概率。在本组病例中未发生与穿刺扩张通道而形成的脑挫伤或血肿形成,我们认为这主要归功于逐步扩张的技术。在进行导引器手术的过程中,可以选择单手持内窥镜,另一手持器械操作;也可以选择让助手持镜,或将内镜以支架固定,以实现术者的双手操作。在实际操作中,我们更倾向选择以支架固定内镜/外视镜,并采用双手双器械操作,从而确保手术的安全、高效的进行。
内镜更适于对病变进行细微、多角度观察和简单处理,而外视镜可以提供相对更充分的空间,更适合处理复杂情况。对于导引器手术,病例的选择很重要。根据我们的经验,较小的病变或位于侧脑室额角的病变,且伴有同侧侧脑室扩大的患者比较适合进行内镜导引器手术。在本研究中,有2例病变位于侧脑室三角区或侧脑室体部,在导引器手术后发生了脑室内的粘连,形成了孤立颞角,经二期脑室镜造瘘手术后治愈。分析原因,术后孤立颞角的发生可能与病变部位的解剖特点有关,如肿瘤位于侧脑室三角区,此处为连接侧脑室体部与颞角的狭窄区域,且脉络丛丰富,导致该部位手术术后更容易发生粘连,进而形成孤立颞角。此外,病变的病理性质及侵袭性也与其在脑室内的活动度、术后孤立颞角的形成有关。根据我们的经验,WHO分级较高或对周围组织有侵袭的病变周边游离程度较低,因此手术切除的难度更大。
综上所述,本研究结果提示,导航辅助下,内镜导引器手术切除部分脑室内肿瘤技术可行,微创高效。尽管初期结果令人鼓舞,但本研究仅为单中心的回顾性研究,且病例数量有限,尚无法提供高级别的循证医学证据。仍需要大规模的前瞻随机临床对照试验来证实这一新颖手术方式的真正价值。
原始出处:
刘磊,赵艺宁,杨佳,姚书敬,杨兵,张家墅,陈晓雷.导航引导下神经内镜导引器辅助脑室内肿瘤切除[J].中国神经精神疾病杂志,2018(06):370-372.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#神经内镜#
37
#肿瘤切除#
52
#脑室内#
49
#内镜#
30
#脑室#
40