Aliment Pharm Therap:炎性肠病患者恢复应答 不妨试试这个方法
2017-05-11 石岩 环球医学
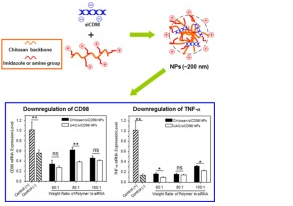
2017年4月,发表在《Aliment Pharmacol Ther》的一项由荷兰科学家进行的研究表明,炎性肠病(IBD)患者使用英夫利昔单抗或阿达木单抗并结合免疫调节剂,能够抑制抗药抗体产生。背景:IBD患者抗肿瘤坏死因子(TNF)治疗失去应答,常常由抗药抗体形成和药效中和引起。已表明添加免疫调节剂能减少免疫原性,使得恢复应答。目的:研究IBD患者中,抗TNF单药治疗添加免疫调节剂能否抑制抗药抗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Pharm#
37
#ERA#
34
长见识了,多谢分享
49
学习了感谢分享!
57
学习了,谢谢
0
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
47
抛砖引玉的作用!
50
炎性肠病患者的防治。
31
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
31
炎症性肠病也是研究热点啊。
24