经眶上外侧入路手术切除大型嗅沟脑膜瘤(附6例报道)
2019-10-17 雷军荣 秦军 罗杰 中国临床神经外科杂志
长期以来,经纵裂入路或双额冠状切口经额下入路是切除嗅沟脑膜瘤的首选手术入路。而有学者认为眶上外侧入路具有开关颅简单、快速、创伤小等优点,可替代翼点入路、经纵裂入路或双额冠状切口经额下入路处理颅前窝底、鞍区、鞍上等部位肿瘤及前循环动脉瘤等。2013年7月至2017年9月采用眶上外侧入路手术治疗大型嗅沟脑膜瘤6例,取得良好效果,现报道如下。
长期以来,经纵裂入路或双额冠状切口经额下入路是切除嗅沟脑膜瘤的首选手术入路。而有学者认为眶上外侧入路具有开关颅简单、快速、创伤小等优点,可替代翼点入路、经纵裂入路或双额冠状切口经额下入路处理颅前窝底、鞍区、鞍上等部位肿瘤及前循环动脉瘤等。2013年7月至2017年9月采用眶上外侧入路手术治疗大型嗅沟脑膜瘤6例,取得良好效果,现报道如下。
1. 资料与方法
1.1 一般资料
6例中,男4例,女2例;年龄43~71岁,平均56岁。肿瘤左右基本对称5例,明显偏于左侧1例。6例均有嗅觉障碍,其中伴有头痛5例、视力减退2例、精神症状1例。术前均行MRI平扫及增强检查,肿瘤最大直径大于5 cm。
1.2 手术方法
取仰卧位,上半身抬高30°,以Mayfield头架固定头部,头部下垂15°~20°,并根据病变位置及大小,向对侧旋转30°~45°。切口位于发际内,起自耳屏前颧弓上方2 cm,沿发际内弧形至中线。肿瘤左右基本对称5例均选择右侧眶上外侧入路,明显偏于左侧1例选用左侧眶上外侧入路。额骨颧突及切口近颞线处各钻一孔,铣刀成形骨瓣,注意额部的暴露需充分,颞部至蝶骨棘下方1 cm能显露侧裂边缘即可,如遇额窦打开需妥善处理。硬膜外磨除蝶骨嵴外侧及额底骨质突起,使蝶骨嵴前方的前颅窝底尽可能平坦。
额部及颞部骨缘间隔2 cm打孔并悬吊硬膜。基底朝向前外侧弧形剪开硬脑膜,打开外侧裂近端及相关脑池释放脑脊液,使额叶尽量松弛。切除肿瘤时,先用双极电凝尽可能多电灼切断肿瘤基底部,充分阻断肿瘤血供以减少术中出血。然后分离肿瘤与额叶之间的间隙,注意保护正常的蛛网膜界面,同时分离肿瘤与视神经、视交叉及大脑前动脉之间的粘连。超声吸引或分块切除肿瘤获得操作空间后,再次电灼剩余肿瘤基底,进一步缩小肿瘤体积,上述操作交替进行直至全切肿瘤。用金刚钻磨除颅前窝底受侵犯骨质,硬膜缺损处以骨膜及生物胶进行修补。关颅时无需引流,应用6-0滑线严密缝合硬脑膜达到“不透水”效果,骨瓣复位,确切缝合肌肉及帽状腱膜
2. 结果
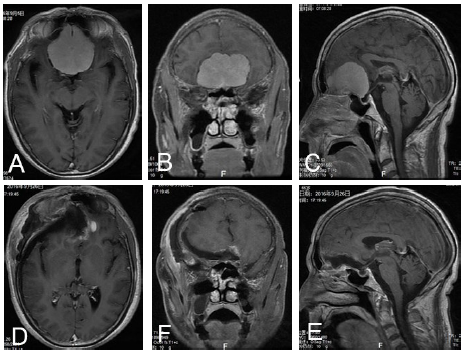
图1 大型嗅沟脑膜瘤经眶上外侧入路手术前后MRIA. 术前MRI增强轴位;B. 术前MRI增强冠状位;C. 术前MRI增矢状位位;D. 术后MRI增强轴位;E. 术前MRI增强冠状位;F. 术前MRI增矢状位位
3. 讨论
3.1 常用手术入路缺陷
嗅沟脑膜瘤是常见的颅前窝底肿瘤,可分为单侧或双侧,也可以一侧为主向对侧生长,当肿瘤较大时,往往累及双侧。本文6例大型嗅沟脑膜瘤亦全部累及双侧。对于嗅沟脑膜瘤的大小分型,尚无统一标准。我们采用高宜录等的标准,将最大直径大于5 cm定为大型嗅沟脑膜瘤。嗅沟脑膜瘤以手术为主。经纵裂入路不能早期阻断肿瘤血供,适用于较小嗅沟脑膜瘤。
对于较大的嗅沟脑膜瘤,有学者主张应用冠状切口经额底入路。经额底入路又可细分为经单侧额底及双侧额底入路,但不管选择哪种入路,经额底入路的基本要求是额部钻孔要足够低,甚至需要打开眶顶,这样容易暴露颅前窝底,可以减少对额叶的牵拉。尽管如此,术中若不能通过释放脑脊液松弛额叶,肿瘤较大时,对额叶的牵拉损伤仍然较重。同时,额窦难免开放,术后脑脊液漏及颅内感染较多。而且,采用双额冠状切口,创伤较大。因为额窦的阻挡,开颅费时费力,关颅亦颇为繁琐,有时遗留额部的部分骨质缺损,影响外观。
也有学者提倡经翼点侧方入路切除肿瘤,但经典翼点入路开颅、关颅较繁琐,且存在额叶显露不够充分及颞叶的无效暴露缺陷。
3.2 眶上外侧入路优点
Juha等采用眶上外侧入路手术治疗颅前窝、鞍旁及蝶骨棘的脑膜瘤,取得良好效果。我们将此入路应用于大型嗅沟脑膜瘤的手术治疗。此入路同翼点入路的区别为:①皮肤切口更小,一般起自颧弓上2 cm,以减少对颞叶的无效暴露;②皮肌瓣一层翻开,避免面神经额支的损伤,减少颞肌萎缩、咀嚼及张口功能破坏或颞下颌关节运动障碍等并发症;③通过增加对眶上外侧的显露而减少处理蝶骨嵴及前床突的步骤。
同时,我们体会,和经典双额冠状切口经额下入路相比,此入路优势更为明显:①手术切口明显缩短,创伤较小;②开关颅程序简化,时间大为缩短;③避免对额叶的牵拉,额叶损伤几率降低;④可以根据需要,适当扩大骨窗,显露外侧裂,打开外侧裂后额叶更为松弛;⑤早期即可显露及保护视神经及大脑前动脉;⑥无需显露矢状窦或结扎矢状窦及大脑镰,避免额叶引流静脉的损伤;⑦对肿瘤基底部的显露更为充分,有利于阻断肿瘤血供;⑧可以早期获得脑脊液的释放,颅内压降低后有利于肿瘤的切除。
3.3 术中注意事项
我们体会应用单侧眶上外侧入路,在充分处理肿瘤基底部,分块切除同侧肿瘤后,可获得空间进一步处理对侧肿瘤。如部分肿瘤生长至大脑镰上方,只需适当切除部分大脑镰即可显露清楚,因此单侧眶上外侧入路完全可以充分显露并切除位于双侧的嗅沟脑膜瘤。术中仍需注意如肿瘤向额极生长较多,开骨瓣需注意额部适当扩大,同时头位较翼点入路而言需向对侧旋转更多。根据需要,此入路还可向颞部适当扩大,显露并可打开外侧裂,会更有利于额叶的松弛及肿瘤的切除。
同时,此入路需要预先磨除前额底的骨棘以以获得更为充分的操作空间,但因肿瘤较大,占位效应明显,颅内压较高,勉强磨除时,对额叶的牵拉较重,此时可以先剪开硬膜,打开脑池释放脑脊液后再进行磨除。肿瘤切除完毕后,钻磨除颅前窝底受侵犯骨质,硬膜缺损处以骨膜及生物胶修补防止脑脊液漏。
综上所述,眶上外侧入路具有创伤小、显露充分、降低肿瘤切除难度及并发症较少的优点,治疗大型嗅沟脑膜瘤效果良好。
原始出处:
雷军荣,秦军,罗杰,牟磊,陈志明,陈亮,潘逸恒.经眶上外侧入路手术切除大型嗅沟脑膜瘤(附6例报道)[J].中国临床神经外科杂志,2018(08):549-551.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#外侧入路#
29
#眶上外侧入路#
41
#脑膜瘤#
48
#手术切除#
34