JBJS:股骨转子部骨折的内固定疗效——髓内钉优于滑动髋螺钉吗?
2013-04-30 JBJS 丁香园
在股骨转子间或转子下骨折的内固定手术治疗中,髓内钉与滑动髋螺钉均表现出良好的良好疗效,但涉及二者的多中心前瞻性随机对照研究却鲜有报道。最近一期的JBJS(Am)上刊登了一篇来自挪威Haukeland大学医院骨科的多中心前瞻性临床调查研究,对髓内钉与滑动髋螺钉治疗转子部骨折的临床效果进行的比较,该研究的证据级别为治疗性研究I级。 该研究对相关病例的评价措施涉及术后疼痛水平,功能改善状况,手术并发症
在股骨转子间或转子下骨折的内固定手术治疗中,髓内钉与滑动髋螺钉均表现出良好的良好疗效,但涉及二者的多中心前瞻性随机对照研究却鲜有报道。最近一期的JBJS(Am)上刊登了一篇来自挪威Haukeland大学医院骨科的多中心前瞻性临床调查研究,对髓内钉与滑动髋螺钉治疗转子部骨折的临床效果进行的比较,该研究的证据级别为治疗性研究I级。
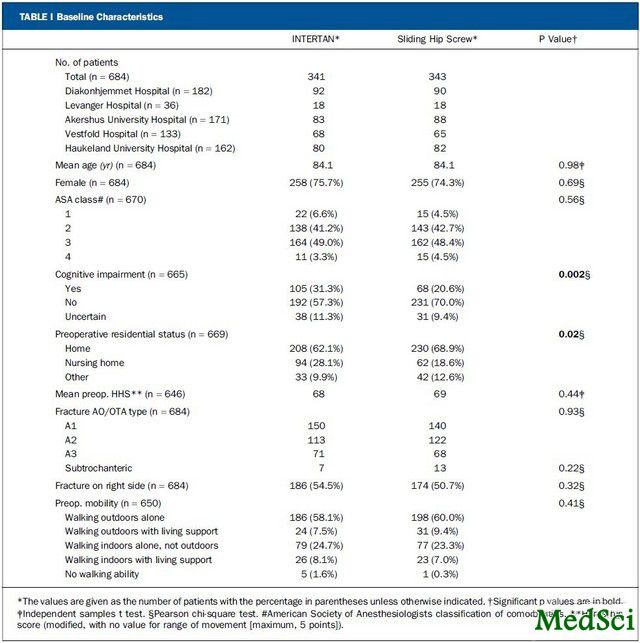
该研究对相关病例的评价措施涉及术后疼痛水平,功能改善状况,手术并发症等多个方面。共有684例老年股骨转子间或转子下骨折患者纳入研究,患者共分为两个治疗组,其中一组采用TRIGEN INTERTAN髓内钉固定,另一组采用滑动髋螺钉固定(更佳具体情况附加或不用转子部稳定钢板)。临床疗效的评价时间点为住院期间、术后3个月和12个月。具体的评价指标包括视觉模拟量表(visual analogue scale,VAS)疼痛评分,计时起走测试,Harris髋关节评分(Harris hip score, HHS)以及EuroQol-5D生活质量评分(EQ-5D)等。另外,还对患者的术中及术后并发症情况进行记录、评价。
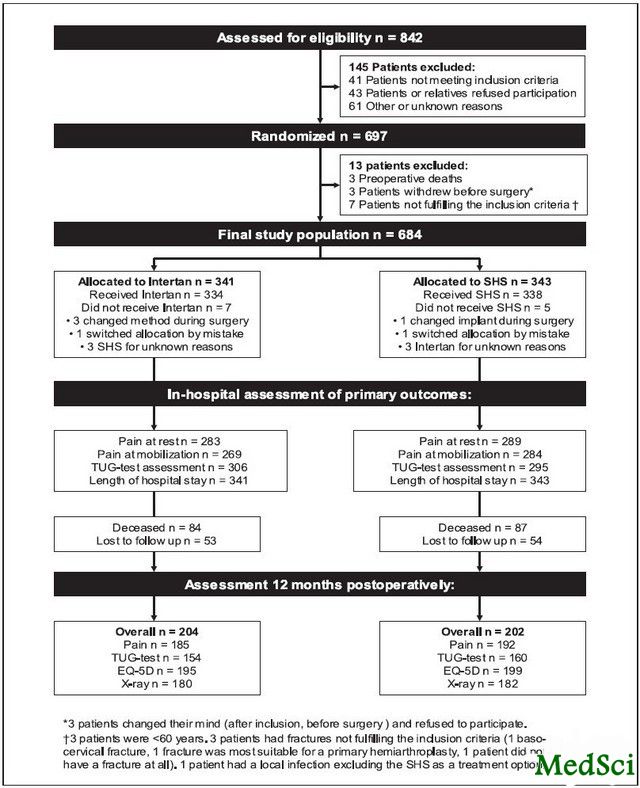
图 1.研究设计流程,SHS,滑动髋螺钉;TUG,计时起走。
表 1.病例的基线特征
研究结果显示,INTERTAN髓内钉治疗组患者术后制动期的疼痛水平更低(VAS疼痛评分:48 vs 52;p = 0.042),但未对患者的住院时间产生影响;在术后12个月时两组间患者的疼痛水平无显著差别。无论骨折类型如何,两组病例在活动功能,髋关节功能,患者满意度以及生活质量评估结果方面,术后3个月及12个月均未见显著差别。两组的手术并发症发生率差异也无统计学意义(滑动髋螺钉组vs髓内钉组:29 vs 32;p = 0.67)。
最终,作者认为,在股骨转子部骨折的内固定手术治疗中,INTERTAN髓内钉与滑动髋螺钉固定术后1年,在患者疼痛水平、功能以及再手术率方面疗效相当。
表 2.疗效评估结果
与骨折相关的拓展阅读:
- 三男子醉酒动粗拳打医护人员 一护士额骨骨折
- 2013AAOS:医疗费用是股骨和胫骨骨折病例住院时间的影响因素
- 2013AAOS:单钢板能为肱骨远端关节外骨折提供足够的稳定性吗?
- JCEM:中山大学陈裕明等发现高脂饮食增加髋关节骨折的发生
- 2013AAOS:全髋置换治疗切开复位内固定术后失败的髋臼骨折
- 2013AAOS:锁骨骨折进行性移位的临床观察 更多信息请点击:有关骨折更多资讯

TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up.
BACKGROUND
Both intramedullary nails and sliding hip screws are used with good results in the treatment of intertrochanteric and subtrochanteric fractures. The aim of our study was to assess whether use of the TRIGEN INTERTAN nail, as compared with a sliding hip screw, resulted in less postoperative pain, improved functional mobility, and reduced surgical complication rates for patients with an intertrochanteric or subtrochanteric fracture.
METHODS
In a prospective, randomized multicenter study, 684 elderly patients were treated with the INTERTAN nail or with a sliding hip screw with or without a trochanteric stabilizing plate. The patients were assessed during their hospital stay and at three and twelve months postoperatively. A visual analogue scale (VAS) pain score was recorded at all time points, and functional mobility was assessed with use of the timed Up & Go test. The Harris hip score (HHS) was used to assess hip function more specifically. Quality of life was measured with the EuroQol-5D (EQ-5D). Radiographic findings as well as intraoperative and postoperative complications were recorded and analyzed.
RESULTS
Patients treated with an INTERTAN nail had slightly less pain at the time of early postoperative mobilization (VAS score, 48 versus 52; p = 0.042), although this did not influence the length of the hospital stay and there was no difference at three or twelve months. Regardless of the fracture and implant type, functional mobility, hip function, patient satisfaction, and quality-of-life assessments were comparable between the groups at three and twelve months. The numbers of patients with surgical complications were similar for the two groups (twenty-nine in the sliding-hip-screw group and thirty-two in the INTERTAN group, p = 0.67).
CONCLUSIONS
INTERTAN nails and sliding hip screws are similar in terms of pain, function, and reoperation rates twelve months after treatment of intertrochanteric and subtrochanteric fractures.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#髓内钉#
46
#股骨#
30
#内固定#
43
#JBJS#
26