Chest:可视化估计的冠状动脉钙化可预测COPD患者心血管疾病!
2018-06-12 xing.T MedSci原创
由此可见,CAC的简单视觉评分在预测患有COPD和不患有COPD的吸烟者CAD事件具有很好的效果。
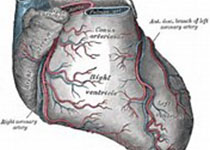
COPD与心血管疾病(CVD)相关,并且为冠状动脉钙化(CAC)提供了更多的预后信息。随着非门控CT扫描在临床实践中的应用越来越多,近日,呼吸领域权威杂志chest上发表了一篇研究文章,研究人员假设视觉韦斯顿CAC评分将如AGAST评分一样可以预测COPD患者冠状动脉事件和冠状动脉病变(CAD)的患病情况和发生率。
研究人员对1875名纳入COPD基因研究的当前和既往吸烟者基于CT扫描测定Agatston评分和Weston评分。研究人员记录了基线心血管疾病和纵向随访心脏事件的发生率,并使用受试者操作特性分析测量CAC分数的准确性,以及使用Cox比例风险分析来估计发生心脏事件的风险。
在基线时发现133例(7.1%)CAD患者。分别有413例(22%)和241例(12.9%)显著的Weston(>7)和Agatston(>400)评分确定的CAC,两种方法具有显著相关性(r=0.84;P<0.001)。超过5年的随访期间,127例(6.8%)患者发生CVD事件。对于预测CAD的患病情况,Weston和Agatston的c指数分别为0.78和0.74,预测CVD的发生率分别为0.62和0.61。调整年龄、种族、性别、吸烟包年、FEV1、肺气肿百分比和CT扫描仪类型后,Weston>7与首次急性冠状动脉事件的发生时间相关(HR=2.16,95%CI为1.32-3.53;P=0.002),而Agtston>400则不是(HR=1.75,95%CI为0.99-3.09;P=0.053)。
由此可见,CAC的简单视觉评分在预测患有COPD和不患有COPD的吸烟者CAD事件具有很好的效果。
原始出处:
Surya P. Bhatt,et al. Visual estimate of coronary artery calcium predicts cardiovascular disease in COPD.chest.2018.https://doi.org/10.1016/j.chest.2018.05.037
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#可视化#
0
#Chest#
27
#动脉钙化#
29
#冠状动脉钙#
33
这个要好好研究.可以再搞一个好课题
56
#EST#
19
#冠状动脉钙化#
36
#COPD患者#
26
#血管疾病#
25
学习谢谢分享
0