J Hypertens:他汀类药物使用对舒张压水平的有利影响!
2017-06-07 xing.T MedSci原创
由此可见,服用他汀类药物与DBP水平显著降低相关。这些效应可以独立观察到,即使在校正心血管危险因素和合并症,以及降压药物的数量。
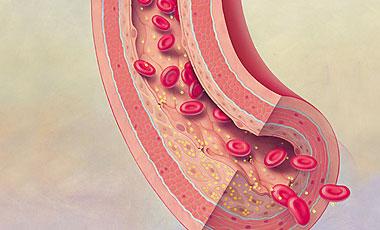
降脂药物被推荐睡觉时服用,尤其是大多数他汀类药物,证据表明夜间血压与心血管事件的风险增加之间具有强烈和独立的相关性。近日,高血压领域权威杂志Journal of Hypertension上发表了一篇研究文章,研究人员旨在评估他汀类药物对夜间血压水平的影响。
研究人员分析了来自于一个大型成年个体的队列的数据,这些参与者在研究人员所在机构进行了家庭、诊所和动态血压监测。根据欧洲指南的建议,研究人员对所有血压指标进行了测量以及设定了血压阈值。研究人群根据他汀类药物使用情况进行分层。
研究人员纳入了5634名成年参与者(女性占48.9%,年龄为60.5±11.6岁,BMI为27±4.6公斤/平方米,诊所血压为144.3±18.4/90.9±12.4mmHg,24小时血压为130.7±13.4 /79.0±9.7mmHg),其中有17.3%的患者接受了他汀类药物治疗,82.7%的患者没有接受他汀类药物治疗。经治疗的门诊患者年龄较大,BMI较高,危险因素和合并症的患病率比那些未经治疗的患者要高(P<0.001)。接受他汀类药物治疗的患者表现出较低的DBP水平,在所有的血压测量中,包括夜间(67.3±9.4 vs. 70.9±9.7mmHg,P<0.001),相比于那些未采用他汀类药物治疗的患者。此外,他汀类药物的使用与24小时[比值比(95%可信区间):1.513(1.295-1.767);P<0.001]和夜间[比值比(95%可信区间):1.357(1.161-1.587);P<0.001]血压控制相关的独立因素,即使在调整了年龄、性别、BMI、糖尿病、降压药数量(模型1)或存在/不存在降压治疗(模型2)。
由此可见,服用他汀类药物与DBP水平显著降低相关。这些效应可以独立观察到,即使在校正心血管危险因素和合并症,以及降压药物的数量。
原始出处:
Tocci, Giuliano;et al. Favourable impact of statin use on diastolic blood pressure levels: analysis of a large database of 24-hour ambulatory blood pressure monitoring.Journal of Hypertension. 2017. http://journals.lww.com/jhypertension/Abstract/publishahead/Favourable_impact_of_statin_use_on_diastolic_blood.97708.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
30
#TENS#
40
#药物使用#
38
#他汀类药#
35
预防一线用药
73
#舒张压#
34
学习了
66
学习并分享!!!
77
继续学习。
59
学习了谢谢分享。
69