Cell Death Dis:治愈新希望!直捣肝癌转移与耐药关键点
2019-09-27 MedSci MedSci原创
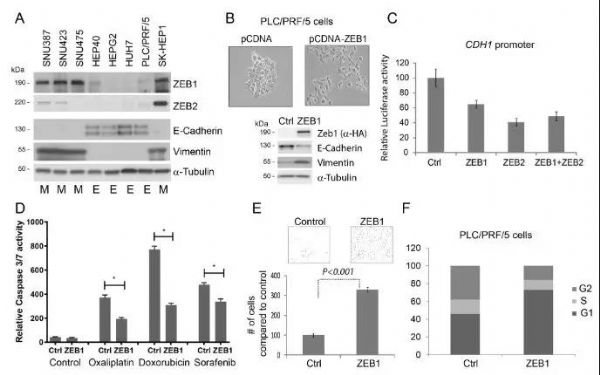
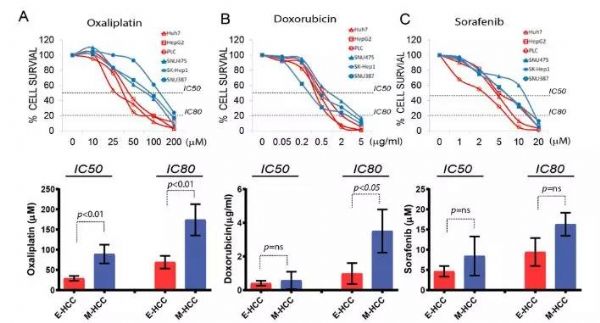
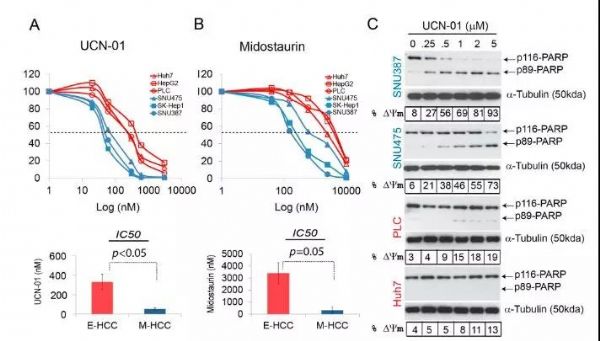
导读:肝细胞癌(HCC)是一种高死亡率的恶性肿瘤,癌细胞易发生转移,导HCC致难以治愈、死亡率极高。临床数据显示HCC转移后对多数化疗药物耐药,手术与放疗亦无计可施。因此,确定可监测HCC转移轨迹的生物标志物及化疗耐药的HCC的靶向药物成为目前肝癌研究领域的重大难题。 近日,英国南安普敦大学的研究人员证明ZEB1是通过驱动癌细胞发生上皮-间充质转化(EMT)上调癌细胞的迁移和侵袭能力,其

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
37
#关键点#
40
#CEL#
32
#Dis#
35
#新希望#
36
#Death#
25
#癌转移#
28
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
0