Ann Intern Med:乳房大、射片多,增加辐射相关乳腺癌风险
2016-01-12 Mechront 译 MedSci原创
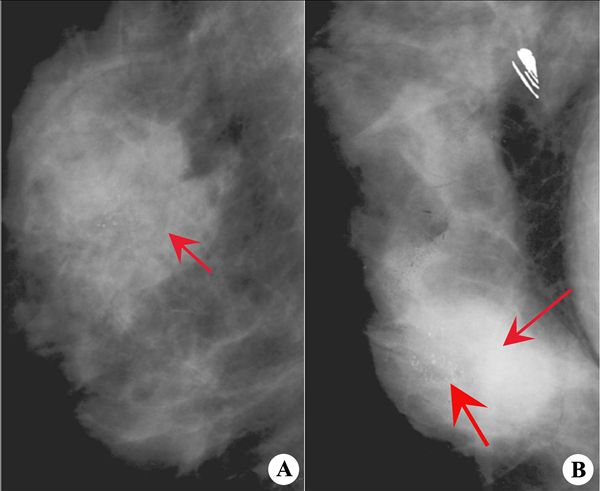
从50岁开始每两年进行一次乳房钼靶检查可降低放射线暴露导致的乳腺癌风险。更大的乳房或隆乳术女性因为辐射的频率和剂量,乳腺癌发病率和死亡率风险更高。该篇发表在内科医学年鉴上的建模研究或会用于更新临床实践建议。重复的数字化乳腺钼靶摄影检查使女性暴露于电离辐射,会增加乳腺癌风险。研究者使用了电脑建模,根据女性筛查频率和剂量的变化,评估数字乳腺X线摄影术中辐射诱发的乳腺癌发生率和死亡率。研究者发现,每年进
从50岁开始每两年进行一次乳房钼靶检查可降低放射线暴露导致的乳腺癌风险。更大的乳房或隆乳术女性因为辐射的频率和剂量较多,乳腺癌发病率和死亡率风险更高。该篇发表在内科医学年鉴上的建模研究或会用于更新临床实践建议。
重复的数字化乳腺钼靶摄影检查使女性暴露于电离辐射,会增加乳腺癌风险。研究者使用了电脑建模,根据女性筛查频率和剂量的变化,评估数字乳腺X线摄影术中辐射诱发的乳腺癌发生率和死亡率。研究者发现,每年进行乳腺钼靶筛查的100000名40-74岁女性中有125例乳腺癌患者和16例死亡,但因为乳腺癌发现的早,也避免了968例死亡。乳房更大或隆胸的女性会受到高于平均辐射剂量的暴露,从而因射线暴露导致的乳腺癌风险增加。年轻时开始开始接受每年筛查也与增加风险。
虽然辐射诱发的乳腺癌发生率与乳腺癌死亡人数相比是非常小的一部分,但是也不能忽视。研究者称,在50岁之前女性开始每年一次的筛查过程中,乳房更大或隆胸的女性其辐射介导的乳腺癌风险是小或正常大小乳房女性的两倍。
原始出处:
Diana L. Miglioretti, PhD; Jane Lange, et al, Radiation-Induced Breast Cancer Incidence and Mortality From Digital Mammography Screening: A Modeling Study, Annals of Internal Medicine, doi:10.7326/M15-1241, published online 12 January 2016.
Biennial mammography screening starting at age 50 may decrease risk for radiation-induced breast cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌风险#
29
#乳腺癌风险#
34
学习了要权衡利害
99
#辐射#
23
#Med#
28