Diabetes:研究发现缺乏维生素D与糖尿病之间的密切关系,缺乏易患糖尿病!
2017-10-24 佚名 Medicalxpress
发表在《糖尿病》杂志上的一项研究,在婴儿期和童年期获得足够的维生素D与降低儿童患1型糖尿病的基因风险的可能性有关。
“几年来,科学家一直在争论维他命D是否降低了胰岛自身免疫性和1型糖尿病的风险。”诺里斯博士说。
1型糖尿病是一种慢性自身免疫性疾病,每年在全球范围内增长3 - 5%。这种疾病现在是10岁以下儿童中最常见的代谢紊乱。在年幼的儿童中,新病例的数量尤其多。高纬度地区的风险似乎更大,从赤道以北更远。
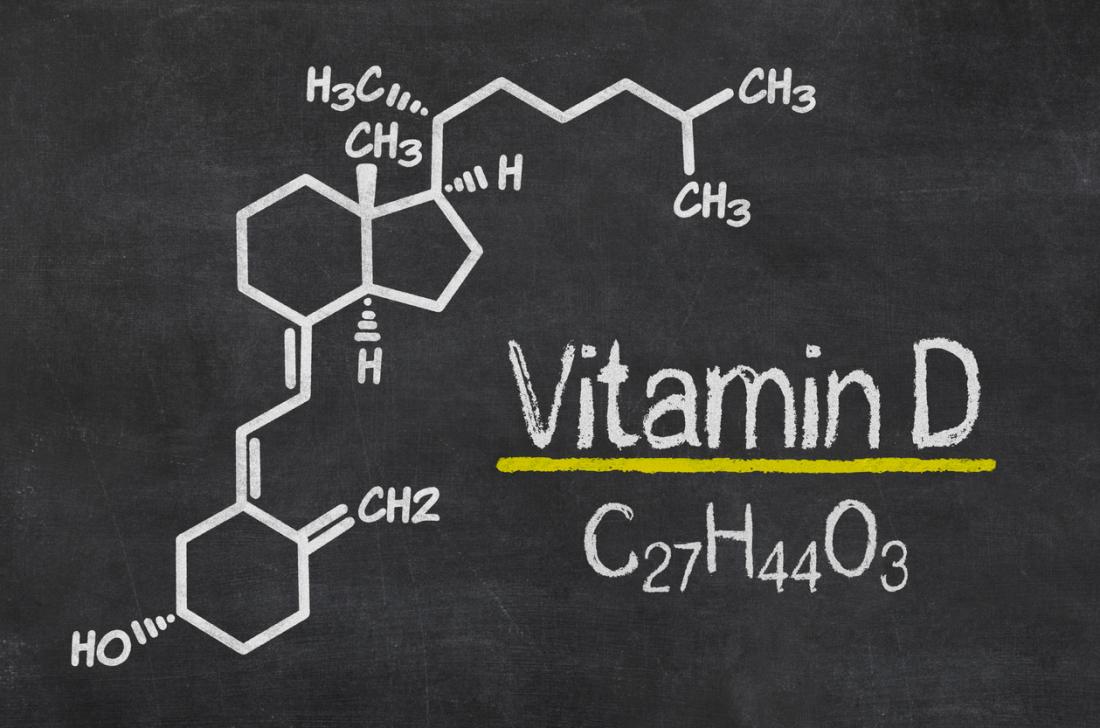
维生素D代表1型糖尿病的候选保护性因素,因为它调节免疫系统和自身免疫性。此外,维生素D的地位因纬度而异。但是维生素D水平和胰岛自身免疫性之间的联系是不一致的。这可能是由于不同的研究设计,维生素D水平的人口变化,或者没有考虑到维生素D通路中暴露和潜在遗传变异的综合影响。
这项研究是由美国国立卫生研究院(National Institutes of Health)的国家糖尿病、消化和肾脏疾病研究所(National Institutes of Health)国家研究所(National Institutes of Health)的国家研究所(National Institutes of Health's National Institute of糖尿病、消化和肾脏疾病)资助的一项大型、多国家研究的研究成果,是糖尿病环境决定因素的一部分。
本研究的目的是在8,676名患有1型糖尿病风险的儿童中寻找1型糖尿病的诱因和保护性因素。
从婴儿期开始,每隔三到六个月就会抽取一个孩子的血液样本,以确定胰岛自身免疫性的存在,以及维生素D的水平。
作者对376名儿童进行了比较,其中有1041名儿童没有得到自动免疫。作者发现,在维生素D受体基因的基因变异的儿童中,婴儿和童年时期的维生素D水平较低,而那些没有发展自身免疫性的儿童则可以自动免疫。
这项研究首次表明,较高的儿童维生素D水平与降低患病风险有显着关联。
“由于这种关联并不能证明因果关系,我们希望未来的研究能够证实维生素D的干预是否有助于预防1型糖尿病,”诺里斯博士说。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
27
#研究发现#
40
#Diabetes#
38
#BET#
34
#密切关系#
40