病例分享:20岁肺癌患者的临终关怀怎么做?关于缓解疼痛,我们存在哪些理解误区?
2018-03-07 刘晶 呼吸界
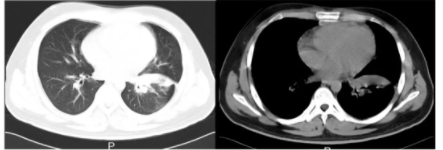
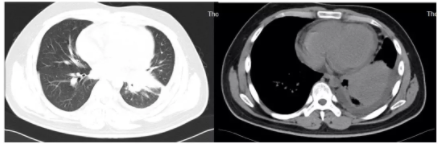
这名患者为20岁男性,在校大学生,既往体健,因咳嗽、咳痰伴胸痛1个月、加重1周入院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







a:¥CnTwb1llNAq¥
88
#缓解疼痛#
31
#肺癌患者#
47
学习了谢谢分享!!
91
#误区#
40
#临终关怀#
65
#临终#
37