Blood:MiR-150下调通过上调FOXP1促进滤泡性淋巴瘤向高级别淋巴瘤转化
2018-09-18 MedSci MedSci原创
中心点:转化FL可下调miR-150,导致FOXP1蛋白上调。上调MYC蛋白可抑制miR-150在转化FL中的表达。摘要:滤泡性淋巴瘤(FL)是一种常见的惰性B细胞恶性肿瘤,临床病程多变,并且其组织学病理可转化成高级别的淋巴瘤,即典型弥漫性大B细胞淋巴瘤(DLBCL)。近期,有研究表明MYC的遗传变异或过表达与FL转化(tFL)相关。但是,FL转化的潜在分子机制尚未完全明了。Katerina Mu
转化FL可下调miR-150,导致FOXP1蛋白上调。
上调MYC蛋白可抑制miR-150在转化FL中的表达。
摘要:
滤泡性淋巴瘤(FL)是一种常见的惰性B细胞恶性肿瘤,临床病程多变,并且其组织学病理可转化成高级别的淋巴瘤,即典型弥漫性大B细胞淋巴瘤(DLBCL)。近期,有研究表明MYC的遗传变异或过表达与FL转化(tFL)相关。但是,FL转化的潜在分子机制尚未完全明了。
Katerina Musilova等人对FL和tFL的配对样本进行miRNAs表达谱分析,发现5个差异性表达的miRNAs。研究人员对其中一个miRNAs(miR-150)展开研究。miR-150在受检的13对样本中的tFL样本中均表现为下调(约3.5倍)。研究人员还发现高水平的MYC通过与miR-150的上游区域结合促进miR-150在tFL中表达。
在B细胞中,MYC介导的的miR-150表达不依赖LIN28A/B蛋白(在髓系细胞中,LIN28A/B蛋白可影响miR-150前体的成熟)。研究人员还发现在tFL中,低水平的miR-150可上调其靶点——FOXP1蛋白;在恶性B细胞中,FOXP1和BCR、NF-κB信号一样是细胞存活的正性调控因子。
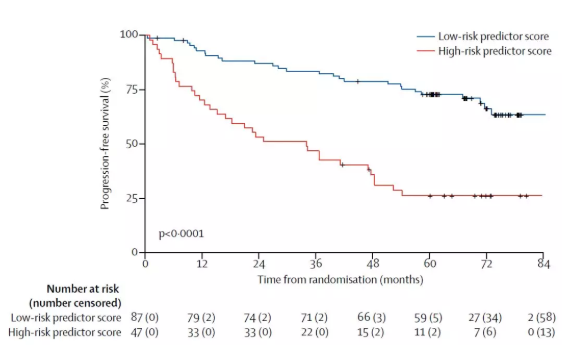
研究人员证实低水平的miR-150和高水平的FOXP1,均与FL总体存活期短相关,提示miR-150可作为一种很好的生物标志物,用于检测福尔马林固定石蜡包埋(FFPE)的组织。
总而言之,本研究揭示了MYC/miR-150、FOXP1轴在恶性B细胞中作为FL侵袭性及其转化的决定因素的作用。
Katerina Musilova,et al. miR-150 downregulation contributes to the high-grade transformation of follicular lymphoma by upregulating FOXP1 levels. Blood 2018 :blood-2018-06-855502; doi: https://doi.org/10.1182/blood-2018-06-855502
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#miR#
27
学习了,谢谢作者分享/
52
学习一下
52
#滤泡性淋巴瘤#
42
学习了谢谢
56
学习了长知识
47
学习了长知识
54
学习了长知识
28
学习了长知识
26
学习了长知识
32