Heart:巧克力摄入与心血管疾病风险
2018-07-31 xing.T MedSci原创
由此可见,巧克力摄入每周<100克可能会降低CVD风险。较高摄入水平可能会抵消巧克力的健康益处并引起与高糖摄入相关的不利影响。
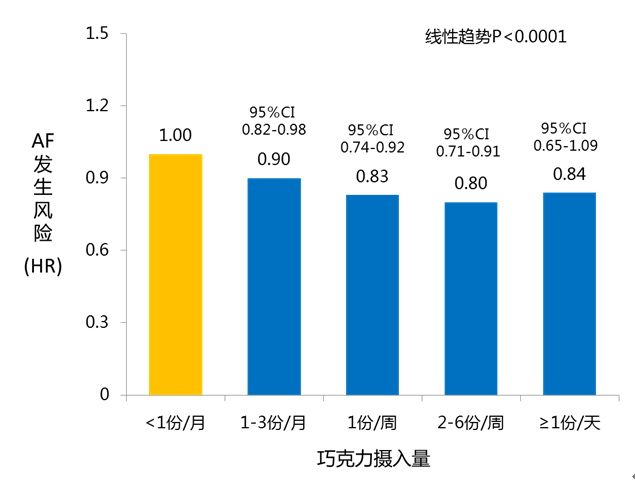
探究巧克力摄入对心血管疾病(CVD)影响的研究并未得出一致的结论。尚未有研究报道巧克力摄入与CVD之间剂量-反应关联的定量评估。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员对评估巧克力摄入相关CVD风险的研究进行了系统评价和荟萃分析。
研究人员检索了PubMed和EMBASE数据库查找截至2018年6月6日发表的文章。使用限制性三次样条来模拟剂量-反应关联。
该荟萃分析纳入14个出版物的研究结果(23项研究,包括405304名参与者和35093例CVD患者)。巧克力摄入每增加20克/周对于CVD相对风险(RR)为0.982(95%CI为0.972-0.992,I2=50.4%,n=18)(心力衰竭:0.995(0.981-1.010,I2=36.3%,n=5);对于总体卒中RR为0.956(0.932-0.980,I2=25.5%,n=7);对于脑梗塞RR为0.952(0.917-0.988,I2=0.0%,n=4);对于出血性卒中RR为:0.931 (0.871-0.994,I2=0.0%,n=4);对于心肌梗塞RR为0.981(0.964-0.997,I2=0.0%,n=3);对于冠心病RR为0.986(0.973-0.999,n=1))。非线性剂量-反应(非线性P=0.001)表明降低CVD风险的最合适的巧克力摄入量为45克/周(RR为0.890; 95%CI为0.849-0.932)。
由此可见,巧克力摄入每周<100克可能会降低CVD风险。较高摄入水平可能会抵消巧克力的健康益处并引起与高糖摄入相关的不利影响。
原始出处:
Yongcheng Ren,et al. Chocolate consumption and risk of cardiovascular diseases: a meta-analysis of prospective studies. Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2018-313131
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很好
60
#ART#
30
#疾病风险#
34
#血管疾病#
32
#HEART#
30
学习了,涨知识了!
59
好消息
66