脱细胞真皮基质复合小牛脱细胞骨修复口腔上颌窦瘘
2019-11-12 李晓宇 伍靖 曹君 华西口腔医学杂志
口腔上颌窦瘘是指口腔与上颌窦之间的上皮相通,由于解剖因素的原因,最常见于上颌磨牙的拔除,尤其是第一、第二磨牙的拔除,其次常见于囊肿及肿瘤摘除术后、牙源性感染等。研究表明,在无炎症的情况下,缺损小于5 mm的上颌窦瘘可自行愈合,大于5 mm的上颌窦瘘则需要干预性的治疗措施。上颌窦瘘的干预性治疗措施主要是外科手术治疗,包括颊侧滑行瓣、腭侧黏骨膜瓣等,但这些方法均有一定的失败率,不能获得理想的治疗效果。
口腔上颌窦瘘是指口腔与上颌窦之间的上皮相通,由于解剖因素的原因,最常见于上颌磨牙的拔除,尤其是第一、第二磨牙的拔除,其次常见于囊肿及肿瘤摘除术后、牙源性感染等。研究表明,在无炎症的情况下,缺损小于5 mm的上颌窦瘘可自行愈合,大于5 mm的上颌窦瘘则需要干预性的治疗措施。上颌窦瘘的干预性治疗措施主要是外科手术治疗,包括颊侧滑行瓣、腭侧黏骨膜瓣等,但这些方法均有一定的失败率,不能获得理想的治疗效果。本研究对上颌骨囊肿或磨牙拔除后引起的口腔上颌窦瘘,采用脱细胞真皮基质材料复合小牛脱细胞骨同期修复缺损及缺损区的牙槽骨,取得了较好的治疗效果。
1. 材料和方法
1.1 研究对象
选取2015年1月—2016年11月在深圳市龙华区人民医院口腔颌面外科就诊需行上颌骨囊肿摘除术或上颌磨牙拔除术的患者,常规行曲面断层片检查,对疑似术后可能与上颌窦相通患者行螺旋CT检查进一步明确,纳入拔牙或囊肿摘除术后口腔上颌窦瘘患者为研究对象。上颌窦瘘的诊断标准:临床检查鼓气试验证实口腔与上颌窦相通。纳入要求:上颌窦瘘缺损大小在5 mm×5 mm以上。共纳入9例研究对象,其中男性4例,女性5例;年龄21~51岁,平均年龄37岁;上颌磨牙拔除患者3例,上颌骨囊肿摘除患者6例,CT检查均显示不伴有上颌窦炎症。术后随访6个月。
1.2 手术方法
拔牙或囊肿摘除术后,在术区与上颌窦相通处,采用骨膜剥离器小心剥离瘘口周围软组织,暴露上颌窦底骨质,将脱细胞真皮基质补片(烟台正海生物科技股份有限公司)放置于窦底,组织面朝向上颌窦,光滑面朝向口腔侧,充分覆盖缺损处周围2 mm以上,骨腔处填塞小牛脱细胞骨(烟台正海生物科技股份有限公司),颊侧滑行瓣缝合消灭创口,4-0丝线缝合颊侧黏骨膜瓣。术后进食流质饮食7 d;同侧鼻腔应用糠酸莫米松鼻喷雾剂50 μg,每天2次,连续使用5 d;2%氯已定溶液漱口;阿莫西林胶囊0.5 g,每天3次;甲硝唑片0.4g,每天2次;告知患者术后2周避免擤鼻涕,3月内同侧避免咀嚼坚硬食物。
2. 结果
9例患者术后切口均一期愈合。术后随访6个月,9例患者口腔上颌窦相通处黏膜均未见瘘道及分泌物,无鼻塞、流脓涕等上颌窦炎症相关症状,临床检查鼓气试验及CT检查均证实创口愈合。2例囊肿摘除患者术后1月内出现同侧面部麻木不适、咀嚼无力感,术后3个月症状逐渐消失。
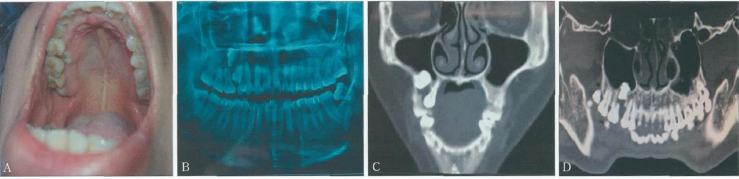
典型病例:患者,女,29岁,2016年6月因右侧上颌第一磨牙松动、擤鼻涕时有液体从口腔溢出就诊,临床检查见右上颌第一磨牙1~2度松动,右上颌第二前磨牙部分萌出于第一前磨牙与第一磨牙之间的腭侧牙颈部,曲面断层片检查显示右上颌第一磨牙近中颊根半数吸收,右上颌第二前磨牙阻生,上方一高位埋伏多生牙突出于上颌窦,冠周形成囊性阴影,与上颌窦无边界。CT检查显示,右上颌埋伏多生牙周围形成囊肿,突出于上颌窦,窦底骨质缺失(图1)。
图1 典型病例术前检查。A:口内观;B:曲面断层片;C、D:CT。
患者入院后在局麻下经颊侧牙龈切口行“右上颌囊肿摘除术、埋伏牙拔除术”,术中见囊腔与上颌窦相通,缺损面积10 mm×10 mm,颊侧骨板部分缺失(图2),第二前磨牙牙根未暴露于囊腔,考虑同时拔除第二前磨牙可引起骨折,暂时保留第二前磨牙,将上颌窦底缺损处周围窦底黏膜小心剥离,修剪后的脱细胞真皮基质放置于窦底,骨缺损处充填多孔小牛脱细胞骨,复位缝合颊侧黏骨膜瓣。

图2 典型病例术中观察
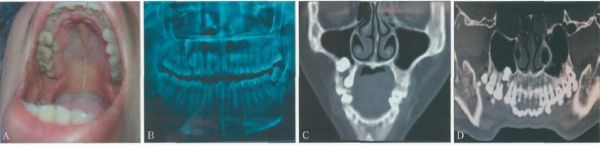
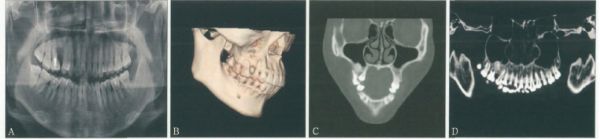
患者术后即刻行右上颌第一磨牙根管治疗,术后1周见创口一期愈合,无上颌窦炎症相关症状,复查曲面断层片显示充填的小牛脱细胞骨无移位,根管充填良好(图3)。术后3个月复查,临床检查见第一磨牙及第二前磨牙无明显松动及叩痛,无鼻塞、流脓涕等症状,曲面断层片检查显示充填小牛脱细胞骨处密度增高(图4)。术后6个月复查,临床检查显示右上颌第一磨牙无松动及叩痛,曲面断层片及CT检查均显示骨缺损充填处愈合情况良好,局麻下拔除高位阻生的上颌第二前磨牙(图5)。
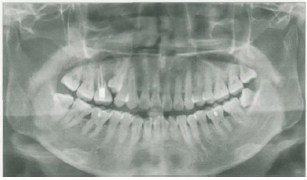
图3 典型病例术后1周曲面断层片

图4 典型病例术后3月曲面断层片
图5 典型病例术后6个月检查。A:曲面断层片;B、C、D:CT。
3. 讨论
由于上颌窦与上颌磨牙根尖之间仅有较薄的骨板,甚至无骨板而仅有黏膜覆盖,在上颌磨牙拔除或磨牙区囊肿摘除术后极易形成口腔上颌窦瘘,尤其囊肿摘除术后的缺损一般较大,并伴有周围骨组织不同程度的破坏,因此在修复口腔上颌窦相通缺损时如果不考虑骨组织缺损的情况,常不能取得理想的治疗效果。既往临床采用的颊侧滑行瓣或腭侧黏骨膜瓣仅仅从软组织覆盖的角度进行了修复,而忽视了骨缺损的修复,因此对于缺损较大的修复常不能取得理想的治疗效果。一些学者采用颊脂垫瓣修复缺损较大的口腔软组织缺损(包括上颌窦瘘的修复),取得了不错的治疗效果,但其无法完成骨缺损的修复,无助于后期的义齿修复。还有一些学者采用移植材料的方法修复缺损,包括植骨、软骨、钛板、钛网等,但各种手段均有自身局限性,包括增加供区创伤、组织坏死、需要二次取出等。
为此笔者设想,如果在修复软组织缺损的同时修复周围骨组织的缺损,并且不需要二次手术取出,将会是一种理想的方法。脱细胞真皮基质是同种或异种脱细胞的表皮基质材料,是用物理、化学等方法将皮肤中的表皮层及细胞成分彻底去除,仅保留真皮中含胶原网架的细胞外基质而得到的。脱细胞真皮基质制作过程中去除了主要免疫活性,故一般不会诱发排斥反应,而保留有正常胶原的三维结构和真皮中含胶原支架的细胞外基质能为组织细胞的再生提供一个良好的支架结构。
脱细胞真皮基质具有一定的厚度,不仅可机械阻隔口腔上颌窦瘘,还保留了真皮与表皮之间的基底膜,故在应用时可形成基底膜与真皮两个面。基底膜面支持移植于其表面的断层皮片的生长,对表皮细胞的分化成熟和移植皮的外观与功能起着非常重要的作用。真皮面有利于在宿主内快速血管化,为成纤维细胞的生长提供良好的支架,有助于脱细胞真皮胶原成分的改建,促使成纤维细胞形成形态结构及排列分布正常的胶原纤维,还具有调节、诱导、促进宿主细胞长入及纤维细胞增生、新生血管和上皮形成等作用。
脱细胞真皮基质最初是作为皮肤移植的替代品,后来在临床上得到广泛应用,包括烧伤创面修复、瘢痕挛缩修复、软组织缺损修复等,其在颌面部组织缺损中也得到了大量应用,如腭裂修复等。近来年在种植领域应用日趋广泛,被证实可有效引导骨再生修复。小牛脱细胞骨与人骨具有相似的化学成分和空间结构,具有一定的机械强度及生物活性,可被降解吸收,提供了良好的生物相容性,有利于新骨的长入,植入体内不仅安全、无毒,还具有一定的骨传导性,而且临床应用简单,无需进行复杂的取骨手术,故能避免额外的损伤,是骨组织工程最为常用的支架材料。
本研究应用脱细胞真皮基质及小牛脱细胞骨,在磨牙拔除或囊肿摘除的同时,修复口腔上颌窦软组织及骨组织缺损,取得了较为理想的治疗效果。本研究使用脱细胞真皮基质及小牛脱细胞骨修复口腔上颌窦缺损,均是在临床及辅助检查排除上颌窦炎症情况下进行的,对于同时伴有上颌窦炎症者,仍建议充分控制上颌窦炎症的情况下再考虑修复缺损。
原始出处:
李晓宇,伍靖,曹君,杨微,武斌,谢春.脱细胞真皮基质复合小牛脱细胞骨修复口腔上颌窦瘘[J].华西口腔医学杂志,2018,36(06):633-637.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#骨修复#
50
#基质#
35
非常受益,很好的研究
66
#上颌窦#
43
#上颌#
0