冠心病应用β阻滞剂严重不规范!报告67家医院1.3万例冠心病患者数据
2019-10-13 朱朱 中国循环杂志
ESC官网近日报告,在正在举行的第30届长城国际心脏病学会议(GW-ICC)上,阜外医院唐熠达和汪京嘉报告了一项入选我国24城市67家医院1.3万例患者的研究。
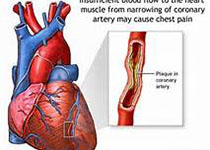
研究发现,大部分急性冠脉综合征和稳定性心绞痛患者出院时没有应用β受体阻滞剂。
而且,即便在应用β受体阻滞剂的患者中,大多数也没有使用最大可耐受剂量。
研究发现,入院前,17%的患者应用β受体阻滞剂;入院后24小时内,β受体阻滞剂的应用比例增至95%。
另外,住院期间,56%的患者β受体阻滞剂剂量没有调整,说明临床医生不确定增加剂量的好处。
唐熠达教授表示,临床医生在用β受体阻滞剂治疗冠脉疾病,尤其急性冠脉综合征患者时,需要特别注意应用时机、剂量和时间。β受体阻滞剂的应用必须个体化。
欧洲心脏病学会(ESC)前任主席Michel Komajda教授指出,ESC指南推荐,几乎所有的急性冠脉综合征或稳定性心绞痛患者接受β受体阻滞剂治疗,而且应该以最大可耐受剂量应用,以确保他们的症状获得最佳控制,并发症和早死风险降到最低。
一项包含9174名欧洲患者的注册研究显示,86%的75岁以下患者出院时应用β受体阻滞剂,≥75岁以上者β受体阻滞剂应用率为78%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
56
#患者数据#
37
#阻滞剂#
36
#β阻滞剂#
29
#冠心病患者#
26
学习了,学习了
57