维持性血透患者10大常规检查,你都知道吗?
2018-08-03 佚名 郑州大学第一附属医院肾脏病医院
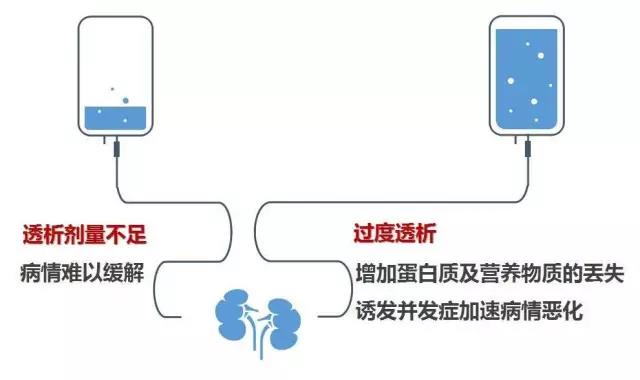
部分血液透析患者在规律治疗情况明显好转后,即认为只要按时透析就行,没必要做一些化验检查。而实际上,却犯了一个很大的错误,因为透析并不能解决疾病本身带来的所有问题,有些问题必须应用药物去干预,而且应定期调整药方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











谢谢了,学习
64
#血透#
29
学习了谢谢分享
58
了解一下谢谢
63
学习了,谢谢分享
68
学习了
49
学习了,谢谢分享。
26
了解一下,谢谢分享!
33
谢谢分享学习
30