J Am Acad Dermatol:皮肤科医生和非皮肤科专科医生治疗痤疮的药物处方的十年变化
2017-07-13 xiaoxiao MedSci原创
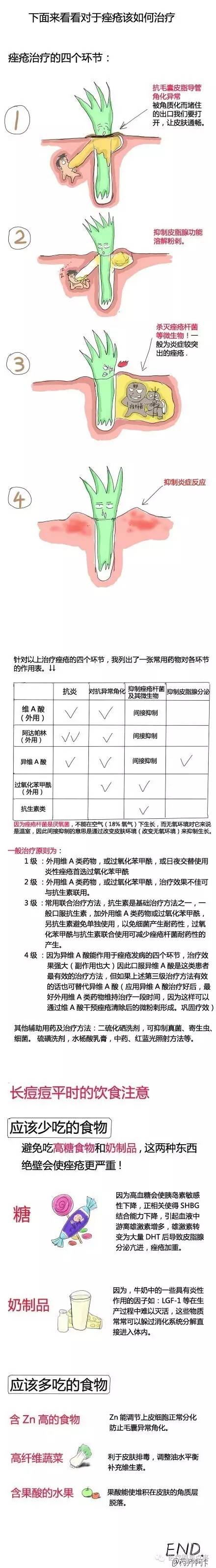
痤疮的发生主要与皮脂分泌过多、毛囊皮脂腺导管堵塞、细菌感染和炎症反应等因素密切相关。痤疮治疗的常用方法包括:(1)局部外用药物——维A酸类等;(2)口服抗生素——四环素类等;(3)口服异维A酸;(4)抗雄激素治疗——口服避孕药复方醋酸环丙孕酮片等;(5)口服糖皮质激素 ;(6)对于不能耐受或不愿接受药物治疗的患者,还可考虑物理治疗,如光动力疗法(PDT)、果酸疗法、激光治疗等。治疗痤疮的方案有很多
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#专科#
39
#专科医生#
32
#ACA#
36
学习了,值得重视
69
#皮肤科#
45
学习了,很不错,点赞
71
学习了受益匪浅。
76
签到学习了很多
73