Hypertension:肾病综合征患者的足细胞损伤促进Ang II的合成和钠水潴留
2019-08-20 MedSci MedSci原创
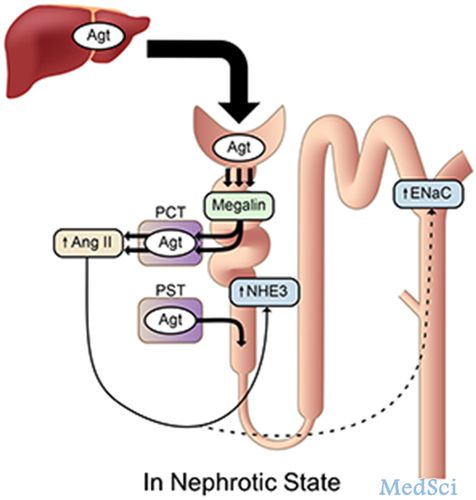
Masahiro Koizumi等人既往发现足细胞损伤科增加肝源性Agt(血管紧张素原)的肾小球滤过率和肾内Ang II(血管紧张素II)的生成,滤过的Agt被近端小管以megalin依赖性方式重吸收。本研究对megalin在肾病综合征过程中肾Ang II的产生和钠处理中的作用进行研究。研究人员建立一个近端小管megalin特异性敲除的小鼠,并将这些KO小鼠与NEP25小鼠进行杂交;NEP25小鼠
本研究对megalin在肾病综合征过程中肾Ang II的产生和钠处理中的作用进行研究。
研究人员建立一个近端小管megalin特异性敲除的小鼠,并将这些KO小鼠与NEP25小鼠进行杂交;NEP25小鼠,可通过注射免疫毒素LMB2诱导足细胞特异性的损伤。
无足细胞损伤时,KO小鼠肾脏的Agt染色明显减少,尿Agt升高。但KO小鼠和对照小鼠的平均肾Ang II相差无几:117(95% CI 101-134)vs 101(68-133)fmol/g组织。随后,研究人员又检测了在足细胞损伤的情况下,敲除megalin对肾内Ang II产生的影响。NEP25对照小鼠的肾Agt染色和肾Ang II(450 [336–565]fmol/g组织)水平均明显增加。Megalin KO/NEP25小鼠的Agt再吸收明显减少,Ang II肾毒性减弱。
与NEP25对照小鼠相比,Megalin KO/NEP25小鼠的分泌的尿钠增加了5倍。蛋白质印记实验显示敲除megalin可减少NHE3和裂解的α/γ形式的上皮Na通道。
综上所述,本研究表明,肾病综合征患者近端小管通过megalin重吸收Agt后转化为Ang II,进而通过激活NHE3和上皮细胞Na+通道促进钠潴留和水肿的发生。
原始出处:
Masahiro Koizumi ,et al.Podocyte Injury Augments Intrarenal Angiotensin II Generation and Sodium Retention in a Megalin-Dependent Manner.ypertension. 9 Jul 2019;74:509–517. https://doi.org/10.1161/HYPERTENSIONAHA.118.12352H
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TENS#
27
#PE#
29
#损伤#
35
#综合征#
38
#Hypertension#
22
学习了
83