JACC:阿司匹林和氯吡格雷低反应性对药物洗脱支架患者的影响
2017-08-22 xiangting MedSci原创
这项研究证实了血小板对氯吡格雷的高反应性与DES后2年缺血和出血结局的强相关性。
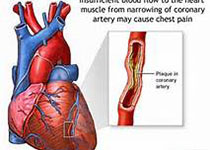
血小板反应性和药物洗脱支架(DES)植入后的长期不良事件之间的关系仍不完全明确。这项研究在对ADAPT-DES(药物洗脱支架双重抗血小板治疗评估)研究2年结局的分析中,试图探讨血小板对阿司匹林和氯吡格雷的反应性和随后结局之间的独立关联性。ADAPT-DES研究是一项关于PCI植入DES后进行常规血小板功能检查患者的多中心登记研究。主要研究终点是明确或可能的支架血栓形成(ST); 其他终点是全因死亡率、心肌梗死和临床相关性出血。2008年至2010年共纳入8582例患者; 46.3%的患者在2年内进行双重抗血小板治疗,无中断。在2年时,92例患者(1.07%)发生明确或可能的ST。连续2年治疗双重抗血小板治疗的患者,对氯吡格雷的高血小板反应性与确定或可能的ST(调整危险比[HR]:2.16; 95%置信区间[CI]:1.27-3.67; p = 0.003 ),心肌梗塞(调整HR:1.35; 95%CI:1.05-1.74; p = 0.02),无临床相关性出血(调整HR:0.74; 95%CI:0.62-0.90; p = 0.002)和全因死亡率(调整后HR:1.36; 95%CI:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
25
#洗脱支架#
32
#反应性#
40
#药物洗脱支架#
40
#ACC#
35
谢谢分享.学习受益匪浅
71